
APA Style
Mohammed Ahmed Alghauli, Shahad Almutairi, Rola Aljohani, Waad Aljohani, Ahmed Yaseen Alqutaibi. (2025). Advanced Subtractive Manufacturing, Micromilling, and Laser Micromachinery in Dentistry: Current Applications, Limitations, and Future Perspectives. Biomaterials Connect, 2 (Article ID: 0013). https://doi.org/10.69709/BIOMATC.2025.138037MLA Style
Mohammed Ahmed Alghauli, Shahad Almutairi, Rola Aljohani, Waad Aljohani, Ahmed Yaseen Alqutaibi. "Advanced Subtractive Manufacturing, Micromilling, and Laser Micromachinery in Dentistry: Current Applications, Limitations, and Future Perspectives". Biomaterials Connect, vol. 2, 2025, Article ID: 0013, https://doi.org/10.69709/BIOMATC.2025.138037.Chicago Style
Mohammed Ahmed Alghauli, Shahad Almutairi, Rola Aljohani, Waad Aljohani, Ahmed Yaseen Alqutaibi. 2025. "Advanced Subtractive Manufacturing, Micromilling, and Laser Micromachinery in Dentistry: Current Applications, Limitations, and Future Perspectives." Biomaterials Connect 2 (2025): 0013. https://doi.org/10.69709/BIOMATC.2025.138037.
 ACCESS
Review Article
ACCESS
Review Article
Volume 2, Article ID: 2025.0013

Mohammed Ahmed Alghauli
malghawli100@gmail.com

Shahad Almutairi
ShahadAlmutairi@taibah.edu.sa

Rola Aljohani
RolaAljohani2@taibah.edu.sa

Waad Aljohani
WaadAljohani@taibah.edu.sa

Ahmed Yaseen Alqutaibi
am01012002@gmail.com
1 Department of Prosthodontics, College of Dentistry, Ibb University, 70270 Ibb, Yemen
2 College of Dentistry, Taibah University, Al-Madinah 41477, Saudi Arabia
3 Substitutive Dental Science Department (Prosthodontics), College of Dentistry, Taibah University, Al-Madinah 41477, Saudi Arabia
* Author to whom correspondence should be addressed
Received: 15 Nov 2024 Accepted: 28 Feb 2025 Available Online: 28 Feb 2025 Published: 25 Jun 2025
Objectives: To comprehensively overview the computer-aided design/computer-aided manufacturing (CAD/CAM) technology, focusing primarily on subtractive manufacturing or Computer Numerical Control (CNC) milling, with special attention to advancements and future requirements. Materials and Methods: A comprehensive web search was conducted in April 2024 across PubMed, Scopus, and Web of Science databases. The inclusion criteria focused on English peer-reviewed studies addressing technological advancements, grinding modes, and limitations. However, non-English articles, case reports, opinion pieces, and studies without substantial technological focus were excluded. Identified studies underwent a two-stage screening process, followed by thematic categorization into three areas: historical development, classification of milling machines, and applications in dentistry. Results: CNC milling technology remains the predominant production method to this day, while interest in additive manufacturing continues to grow. The 5-axis milling machines are the most advanced in dentistry; however, higher axes of milling have yet to be introduced. Recent advancements have seen hybridization, incorporating integrated lathes or 3D printing, as explored by manufacturing companies and researchers. Conclusion: Understanding the subtractive manufacturing pros and cons is crucial to addressing the challenges associated with material waste, time-intensive production, and accuracy concerns. Additive manufacturing or lathe technology with 5-axis milling machines creates new opportunities for beneficial hybridization. Furthermore, the compact and steady design of milling machines, combined with the integration of AI and innovative manufacturing techniques, has the potential to significantly enhance the efficiency, speed, and quality of dental parts production. This promotes remote monitoring, simplifies CAD/CAM processing steps, ensures ergonomic posture, and facilitates a fluent workflow.
Digitization has become the new reality in everyday dental practice, revolutionizing dental procedures, in particular, restorative, prosthetic, surgical, and orthodontic approaches. This advancement improves precision, efficiency, and simplicity, while also providing standardized approaches [1,2]. The digital workflow offers conservative approaches in all dental fields, including orthodontic surgery [3], virtual implant planning, and guided implant placement [4], especially for delicate and thin restorations that cannot be created using conventional manual techniques [5,6,7]. In addition to avoiding complex traditional clinical procedures and laboratory steps, this technology provides acceptable, less stressful, and more comfortable treatments [8], resulting in enhanced patient oral health-related quality of life [1]. The Computer-aided design/computer-aided manufacturing (CAD/CAM) technology encompasses several steps in the production of dental parts, namely data acquisition, CAD software designing, and the actual production (CAM) of the dental parts, Figure 1. The CAM process can be achieved using three main technologies. Firstly, robotics is the least utilized CAM technique and is primarily employed for orthodontic purposes [9]. It should be noted that robotics in the dental field is still in its early stages [10]. The second CAM technology is subtractive manufacturing, also known as computer numerical control (CNC) milling. This technology is the primary and most commonly used method to date [2,5,11]. Lastly, additive manufacturing (3D printing) involves the production of parts layer by layer [2]. Apart from the growing adoption and application of 3D printing in several dental fields, it hasn’t reached the simplicity, availability, and popularity of the CNC milling technology. Therefore, this review aims to examine subtractive manufacturing, particularly CNC milling, by providing a comprehensive analysis of advancements in CAD/CAM technology. The review highlights emerging innovations and identifies future requirements within the field.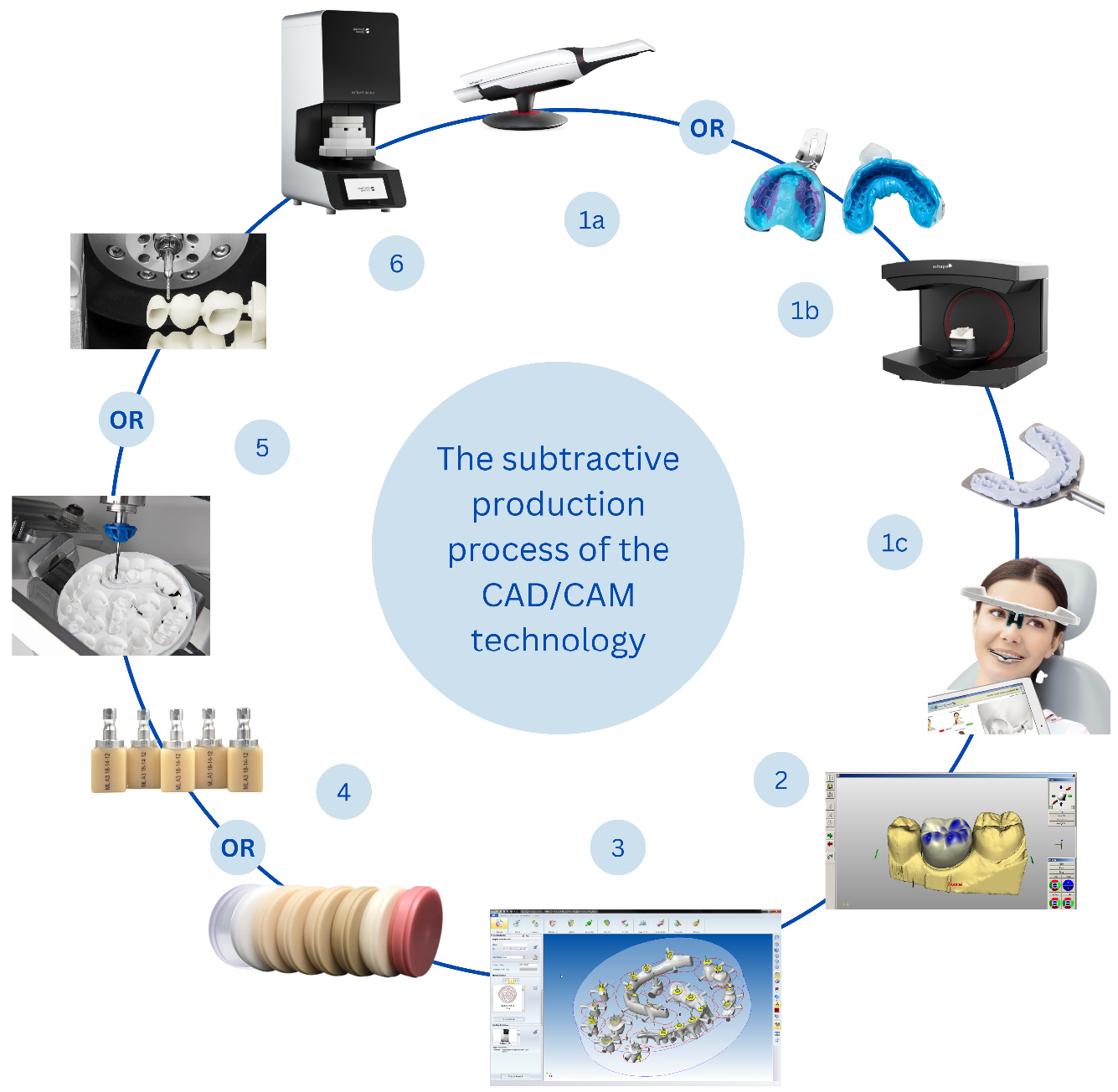
A comprehensive literature search was conducted across three major databases: PubMed, Scopus, and Web of Science, encompassing publications up to April 2024. The search strategy was meticulously crafted to identify all relevant records that evaluate or report on subtractive manufacturing technologies in dentistry. The search terms comprised a combination of keywords and Boolean operators, including “subtractive manufacturing,” “dental milling,” “CAD/CAM dentistry,” “milling machines,” and “dental prosthesis.” Search filters were applied to include only peer-reviewed studies published in English. The search strategy underwent iterative refinement to ensure comprehensive coverage of the topic. Inclusion criteria were established to focus on peer-reviewed studies, reviews, and reports that directly addressed subtractive manufacturing technologies and their applications in dentistry. Studies were included if they examined technological advancements in terms of system evolution, number of milling axes, grinding modes, and associated limitations. Exclusion criteria were implemented to omit non-English articles, case reports, opinion pieces, and studies lacking substantial technological focus. Identified studies were screened in two stages: Title and Abstract Screening—initial selection based on relevance to the predefined themes, and Full-Text Review—detailed assessment to ensure alignment with the inclusion criteria. The first web search in all databases (PubMed, Scopus, Web of Science, and Cochrane) resulted in 3249 records. These records were downloaded to the EndNote reference manager (EndNote 20.5X, Clarivate) for further processing. Sixteen records were initially removed; they were conference abstracts. Fifteen studies were duplicates and hence omitted from the library. The title and abstract of 1241 records were screened for illegibility, 247 seen relative to the topic. Moreover, a manual web search was conducted on websites such as Google Scholar to broaden the search. Ultimately, 193 studies were included, among which 28 records focused on milling technology in dentistry, 31 records focused on micromilling and laser micromachinery, and the rest were interested in milled dental products, milled dental materials, and applications in the dental fields. The included records were systematically categorized into four primary themes. The first theme, Historical and Developmental Aspects, focused on examining the evolution and advancements in subtractive manufacturing technologies. The second theme, Classification of Milling Machines, involved identifying and categorizing the various types of milling machines utilized in dental applications. The third theme, Applications in Dentistry, explored the diverse roles of subtractive manufacturing in dental restorations, prosthetics, and other clinical applications. Finally, the fourth theme, Materials Employed, analyzed the types of materials processed through subtractive techniques and their implications for dental outcomes.
Numerically controlled (NC) manufacturing has a history spanning almost 80 years. The origin of NC milling can be traced back to the period between the 1940s and 1950s. The evolution of computer manufacturing in the 1960s was further propelled by the necessity for more accurate products, surpassing the limitations associated with traditional manual fabrication. The technology operates based on a series of commands that control the cutting tools and dictate the magnitude and direction of movement [12]. Accordingly, the definition of modern CNC milling is the production of parts by cutting through prefabricated blocks or discs of particular material until reaching the desired predesigned form [13]. The process needs CAD 3D digital pattern, CAM software, a milling machine, and prefabricated discs or blocks. The CAM software transforms the CAD model into a toolpath for the CNC machine, performing complex calculations to generate a sequence of commands [14]. In the field of dentistry, a significant milestone was reached in 1971 when Prof. François Duret introduced the fabrication of dental crowns using optical impressions [15,16]. This groundbreaking development laid the foundation for future advancements in dental CAD/CAM technology. The first clinically applicable system was the CEREC in-office system in the 1980s, which was to produce single ceramic intracoronal restorations [17], developed by Mörmann and Brandestini [18]. This device played a crucial role in the advancement of dental CAD/CAM technology by facilitating the development of intraoral scanners and in-office dental milling machines [16]. Building upon these innovations, Dr. Matts Anderson further expanded the application of this technology to include metal restoration fabrication [19]. Figure 2 refers to a visual representation of these developments.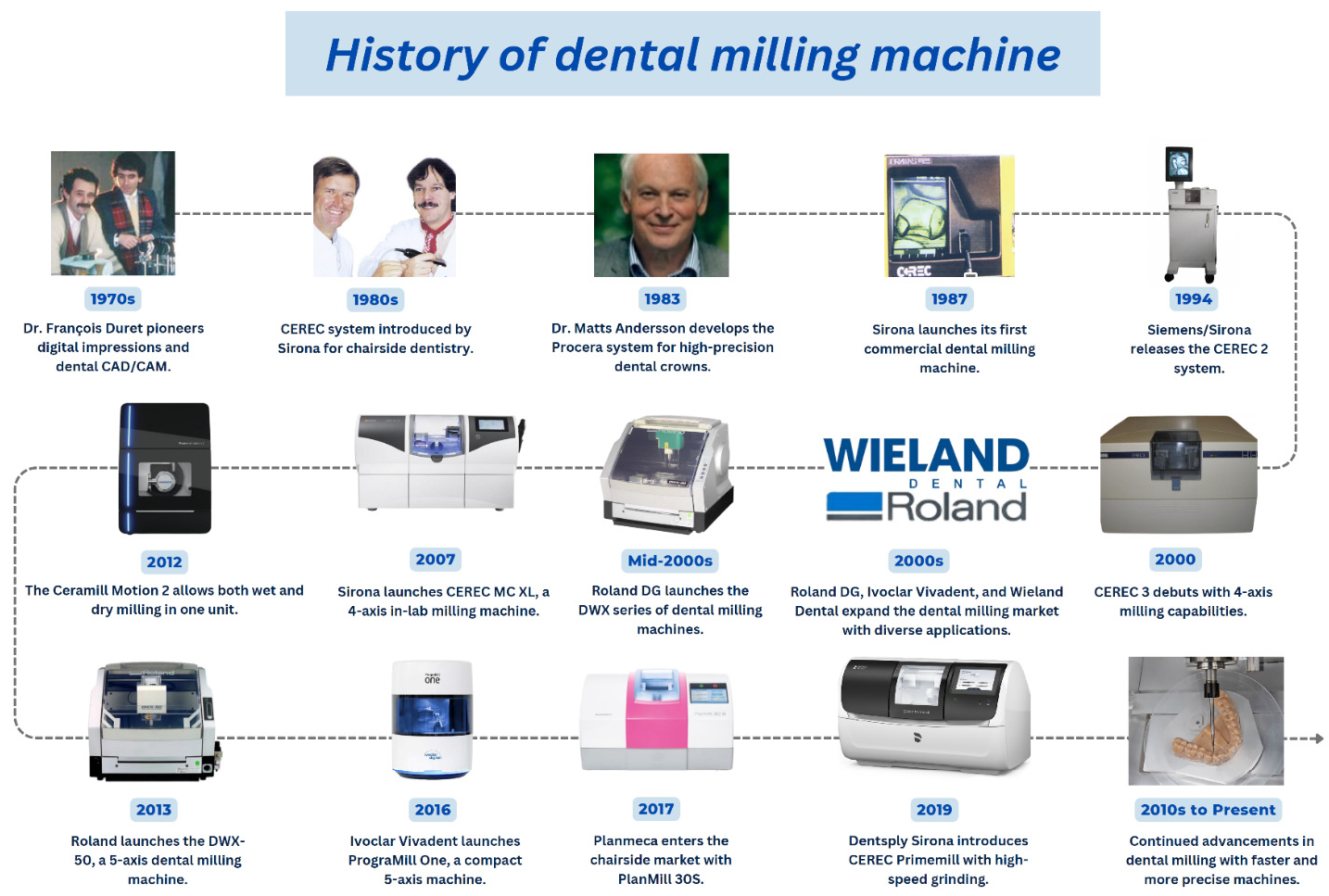
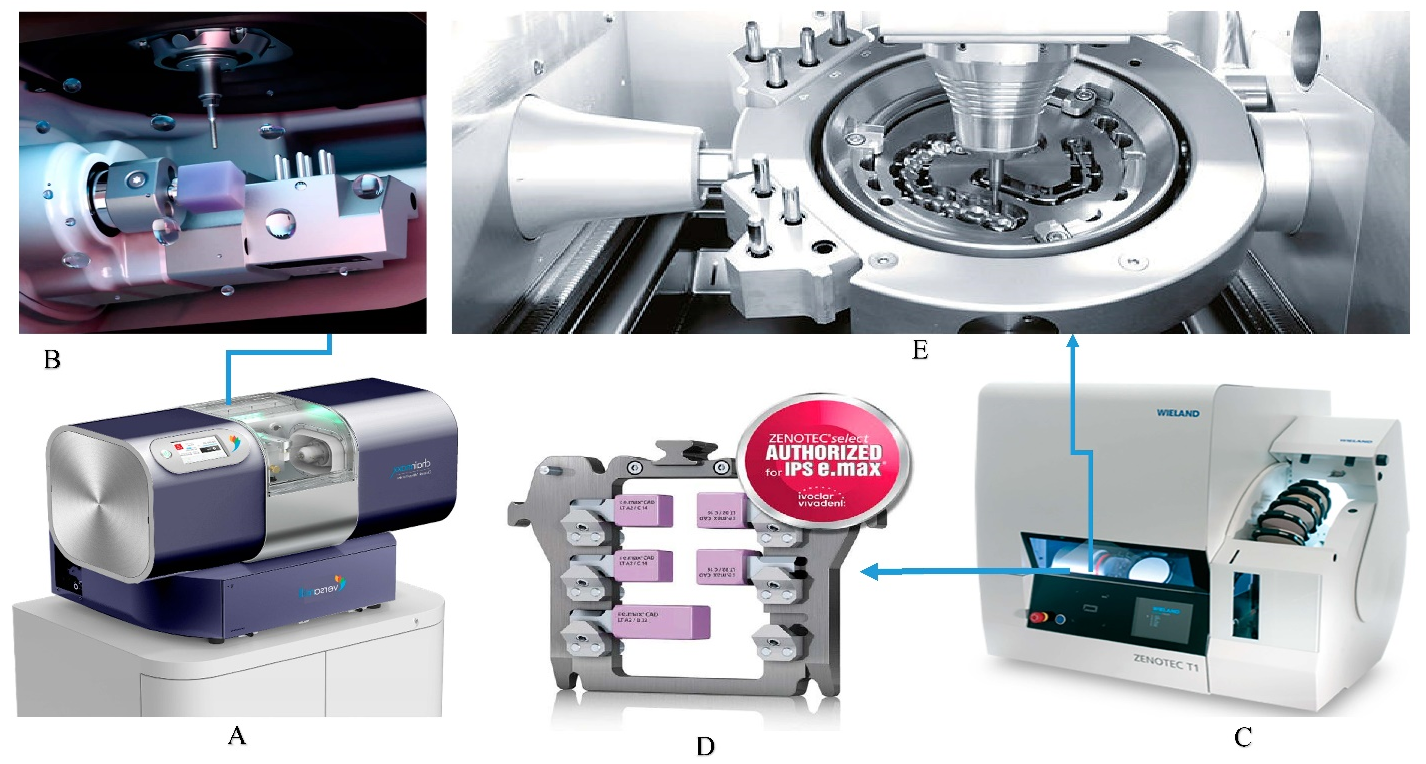
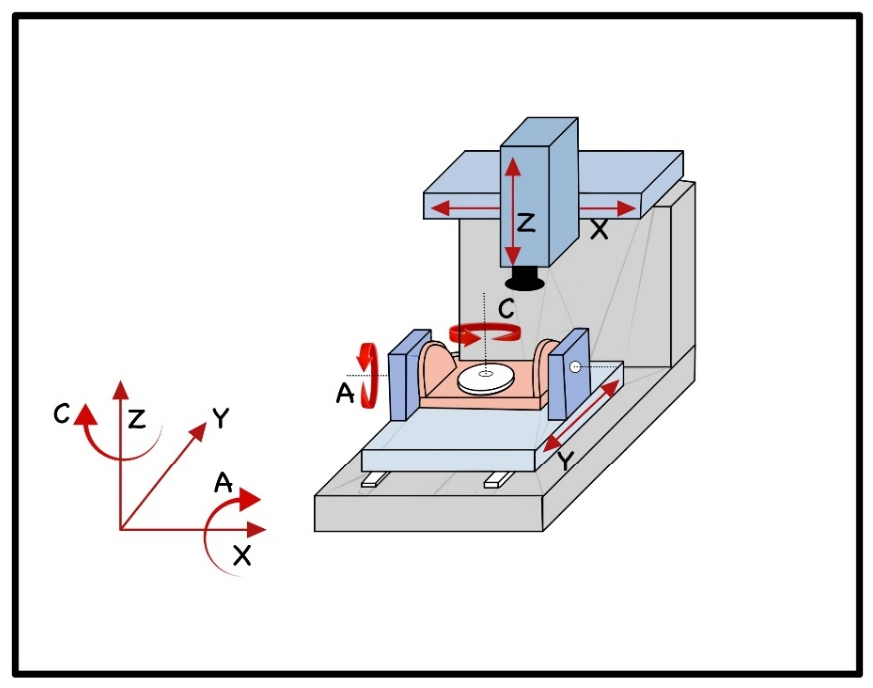
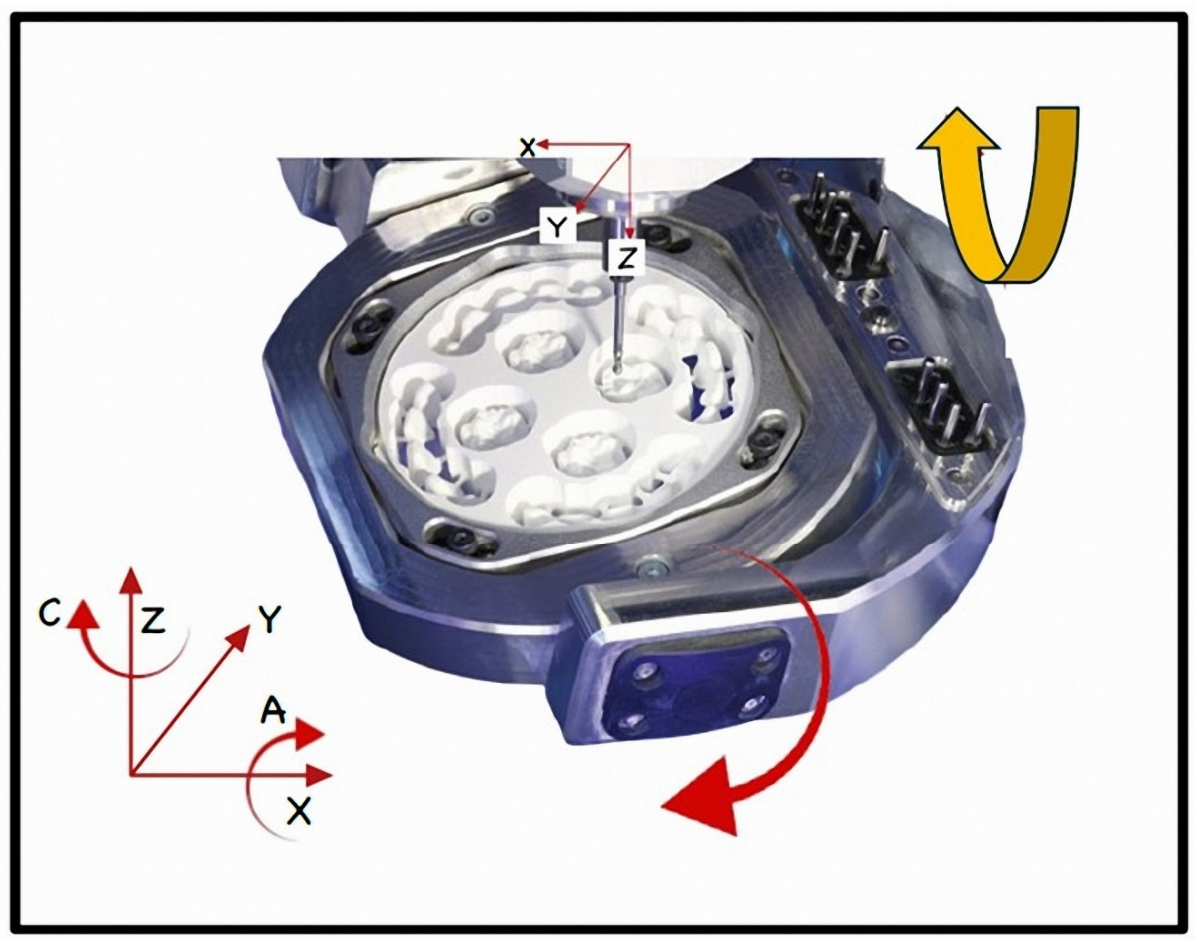
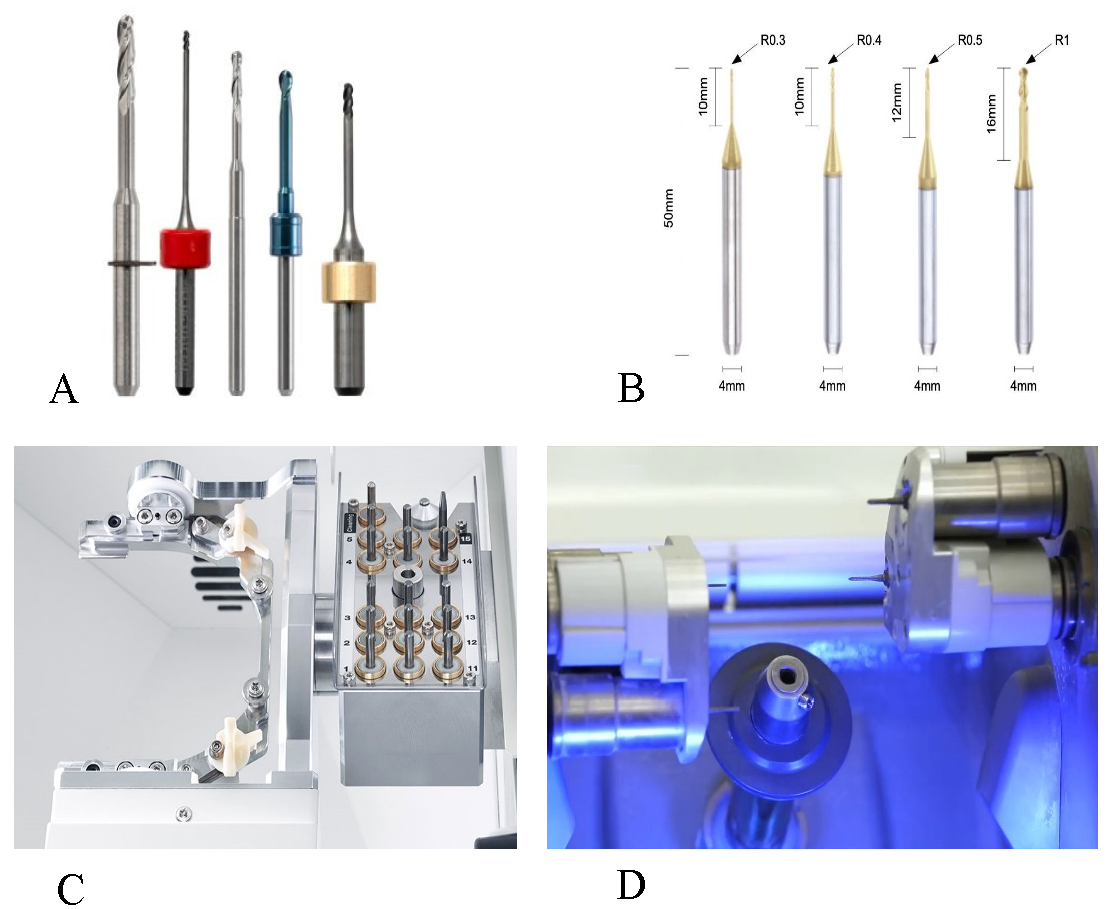
4.1. According to the System Used The CAD/CAM system used in the dental field is roughly classified into in-office and in-lab systems. In this review, the differentiation involved the milling machines and their advancement. In general, the main differences meet the size of the machines and their applications, particularly the degree of advancement, the ability to mill various materials, and the ability to mill complex and large prostheses. These differences shrank gradually with the continuous development of technology. For instance, the chairside CEREC Prime mill is; a 4-axes milling machine that can grind blocks up to 70 mm to produce inlay, onlay, crowns, veneers, screw retained crowns for implants, multilayer abutment, and bridges. The machine can grind zirconia and other ceramic materials from various manufacturers. The machine possesses many features and options, including milling modes and speed protocols, which can finish a single restoration in 5 minutes at the highest speed [20]. Figure 3 shows the differences between chairside and laboratory systems with their modern interlacing. 4.1.1. In-Office (Chairside) CNC Milling There are only three known milling machines that belong to complete chairside systems: the father of all and the leader of the chairside, the CEREC system, Planmeca, and Fastmill.io from Glidewell. Although Fastmill.io intraoral data acquisition devices featuring third party intraoral scanners from Medit. Several other chairside machines that are highly advanced have been introduced recently, such as the 5-axis Programill one from Ivoclar, among others that apply third-party data-acquisition devices and designing software [21]. Figure 4 revealed the differences between chairside and laboratory milling machines. A detailed description of the available in-office milling machines is listed in Table 1, and an extended version of other milling machines capable of in-office production is listed in Supplementary Table S1 (available online). The most commonly used chairside milling machines, as a complete system or depending on third-party data acquisition and CAD software, with brief descriptions (more machines are in Supplementary Table S1). 4.1.2. Laboratory CNC Milling System The laboratory milling machines were inspired by the first CEREC system in the 1980s. However, the complete laboratory system was first introduced in 2000 with the laboratory scanner and CAD software [17]. The main purpose is to manufacture complex restorations that could take a longer time via chairside, use high-strength materials, or need long grinding and processing time, indicating their laboratory manufacturing [25], Figure 4, and Supplementary Table S2 (available online). For single restorations, a chairside system could be preferable to save time and reduce visits [26]. 4.2. Classifications According to the Number of Axes The classification and definition of the number of milling axes in dentistry is very ambiguous and differs from the classifications applied in other industrial realms due to differences in the machine’s components, design, and purpose, Figure 5. Generally, in dentistry, the classification should refer to the spindle axes and the object base movements, Figure 6. CNC machines in dentistry are 3-, 4, or 5-axis milling machines. In 3-axis milling, the tools move in three dimensions (x, y, and z axes) based on the pre-calculated path, or the spindles and base move in two axes and have an extra rotational move. The simplicity and reduced time for calculation and milling are what characterized the 3-axis machines [19]. Large and complex prostheses are not typically produced using 3-axis machines [13]. Examples of such machines include the first introduced machines from inLab (Sirona), Lava (3M ESPE), and Cercon brain (DeguDent) [19]. Four-axis milling machines add another direction of movement, primarily characterized by a single-direction rotational movement of the object base. This feature is particularly useful for shaping larger blanks and creating extensive frameworks [13]. The Planmeca PlanMill 35, and the last introduced Primemill from Sirona, are good examples of a 4-axis chairside machine [20]. Typical and widely used 4-axis laboratory milling machines are Zenotec mini (Wieland-Imes) [19], CEREC inlab MC XL [27], and Ceramel motion 2 from Amman Girrbach, besides a lot of other laboratory machines support 4-axis milling such as DWX-4 from Roland, 88mill from 88dent, and Z4 from vhf. The available milling machines are listed in Supplementary Tables S1 and S2 (available online). The transition to 5-axis milling machines includes adding rotating movements in two different directions of either the milling tool or the blank. This includes X-, Y-, and Z-axis translation, along with A- and C-axis rotation (Figure 4), enabling the creation of complex geometries and smoother external surfaces [13]. In industrial settings, these machines are essential for fabricating intricate parts like curved holes [13]. In dental applications, 5-axis machines excel in crafting complex shapes, such as acrylic denture bases [28]. The adaptation of digital complete dentures favors the 5-axis milling rather than the pack-and-press conventional method [29]. Today, 5-axis milling machines are the most widely introduced in the dental field, particularly in the literature data. Some of the modern examples include Zenotec select and T1 from Wieland, DWX-50, Everest Engine (KaVo), and HSC Milling Device (etkon), more examples are listed in Table S2 (available online). Dental restorations and prostheses quality doesn’t solely depend on the number of milling axes; rather, it’s more about how the work-pieces are processed and the execution of the CAD-designed milling path [19]. Nevertheless, the number of axes of the milling machines is indeed a ruling factor on the trueness, precision, and surface characteristics of the end product [30]. The comparison of the 3-axis with advanced milling machines showed a significantly higher marginal gap and higher surface roughness of the produced restorations [31]. For simple dental restorations such as lithium disilicate crowns, 3- and 5-axis milling machines both produced crowns with acceptable marginal discrepancies. However, the marginal gap was higher in 3-axis machines [32]. Planmill 30s or 40s or CEREC MCX produced molar crowns with comparable marginal, axial, and occlusal gaps [24]. Planmill 30s has a 3-axis spindle and rotating object base, while the latter two machines have two spindles moving simultaneously within 3-axis capability, confirming the non-significant effect of spindle numbers [24]. Nevertheless, intracoronal restorations of a 5-axis milling machine could show better adaptation than those of a 3-axes milling machine that produced restorations in laboratory study, and both showed discrepancies <100 µm [33]. There is a significant correlation between the number of milling axes, the surface of the restoration measured, and the optical impression device on the marginal and internal fit of inlay/onlay restorations; these differences are more prominent with retentive designs [34]. The role of 4-axis over 3-axis CNC milling shines more in laboratory-produced dental parts [35], exhibiting good potential to produce implant-supported frameworks from titanium and zirconia. The accuracy of fit matters more than the type of material in terms of framework passivity [36]. Moreover, the 4-axis milling was applied successfully for the production of detailed, thin, and delicate restorations, such as resin-bonded fixed dental prostheses [37,38], customized post and core crowns [39], and full arch prostheses [40]. However, for full mouth rehabilitations, the single crowns could be twice more accurate than the full arch single prostheses, the accuracy of fit was dependent on the type of restoration, the location of the tooth, and the surface being measured [40]. The 5-axis milling machine showed high trueness of delicate restorations as partial crowns when compared with the original CAD design [41]. The marginal discrepancies and cement space were lower for the 5-axis compared with the 4-axis milling machine [42]. Research comparing two distinct milling units, while utilizing identical scanning systems and CAD software revealed that 4-axis milling units exhibited lower precision in fit when compared to their 5-axis counterparts. This difference was especially noticeable in terms of the occlusal marginal gap and axial internal gap [33,43,44]. The 5-axis machines offer the advantage of milling steep walls, narrow angles, and undercuts from various orientations [11,45]. Furthermore, the dimensions and design of the milling unit’s rotary instrument are critical in influencing the adaptation quality of restoration [11,45,46,47,48,49,50,51]. Any surface intricacies smaller than the diameter of the milling rotary tool can potentially result in compromised restoration accuracy, particularly at the line angles of the preparation [11,47,52,53]. Nevertheless, all dental milling machines inherited limited access to mill complex prosthetic parts and different geometrical structures, which is still reflected in the product’s accuracy [2,44,45,54]. In industry, more advanced machines are applied with 6 to 12 milling axes, these machines differ in form and shape and purpose to be adopted for dental practice. The 9-axis milling machine comprises a 5-axis milling machine for the surface and a 4-axis lathe for inner structures. This type of milling device can give a future insight into the customized milling of intricate dental parts with inner geometrical designs such as dental implant fixtures and superstructures. The 12-axis laser micromachinery has been available since the beginning of the third millennium [55]. The 6-axis milling machine is the closest to be adopted for dental applications, sharing the same design as 5-axis machines with an extra vertical transverse movement of the holding base as depicted in Figure 7. 4.3. Classifications According to the Mode of Milling The majority of milling machines offer one of two options: wet milling or dry milling, such as VHF milling machines. Recent technologies have incorporated both options in the same milling unit, such as the 5-axis W52 milling machine from DERBAG and Zenotec select hybrid. The application of each grinding technique depends mainly on the material being processed [57], and the operator’s preference [58,59]. 4.3.1. Hard Milling or Wet Processing Hard milling is predominantly employed for hard materials grinding, such as metals, and densely sintered zirconia [60]. It demands a robust CNC system capable of handling the intense cutting forces necessary for accurately shaping hard materials [13,60]. A considerable amount of heat is generated during this process, particularly when working with materials that have low thermal conductivity, such as titanium and zirconia [12,61]. This heat can reduce the lifespan of milling tools and potentially affect the integrity of the milled material [61]. Therefore, continuous cooling systems are imperative in this method to prevent any overheating issues [13]. The challenge of CNC milling depends on the respective material [5]. Materials, such as lithium disilicate, composite resin, zirconia-reinforced lithium disilicate, zirconia-reinforced lithia silicate, polymethyl methacrylate, and resin matrix ceramic provided in prefabricated blocks or discs are processed by wet milling mode to avoid heat generation and cracking of the produced parts [11,62]. Moreover, fully sintered zirconia blocks and discs are preferred to be wet ground to avoid cracks and fracture, titanium discs wet milling is also the protocol of choice to avoid overheating and damage to the milling tools, and Co-Cr alloys can be both dry and wet milled relied on the installed system [11]. Wet processing has shown quite an improvement in the life span of cutting tools and in preventing undesirable dust generation [63]. Despite being highly effective, hard milling is a time-intensive process and may lead to undesirable phase transformations in materials like zirconia, which could result in surface micro-cracking and thermal degradation [64,65,66]. This effect on the zirconia surface is also dependent on the cutting tools and the material’s inherited properties [67]. 4.3.2. Soft Milling or Dry Processing This grinding approach is indicated for relatively low-hardness materials or those that imply dry milling [13,60], presintered zirconia, Co-Cr alloys, and wax are typical examples of dry-milled materials [11]. Soft milling has been adopted by numerous manufacturers due to its ability to streamline the milling process and enhance time efficiency. Soft milling in the recently introduced devices is very impressive, such as Primemill for chairside procedures, grinding a single zirconia crown efficiently in less than 5 minutes [20]. Following the milling process, the material undergoes sintering, resulting in a shrinkage of the final product. The percentage of post-processing volumetric change depends on the material itself, comprising approximately 23% for zirconia [68], while it is much lower for other materials, for instance, the shrinkage of lithium disilicate is about 0.2%–0.3% [69], However, these changes do not require any manual adjustments before milling, as the materials are pre-programmed into the device system. This grinding system expedited milling operations, decreased cutting forces, prolonged tool durability, and posed the potential for surface quality enhancement and the absorption of moisture elimination in discs and blocks, thereby eliminating the necessity for pre-sintering drying protocols [19,64,70]. Nevertheless, this method does carry the risk of increased dimensional discrepancies compared to hard milling, as noted in both laboratory and clinical studies [13,69]. Wet-ground zirconia exhibited better mechanical properties than dry-milled specimens [63]. However, wet milling using impregnated water should be avoided, as it leads to the saturation of alumina particles in the ground zirconia, negatively affecting the translucency of zirconia restorations [59]. Despite these challenges, ongoing advancements in the soft milling process are continually improving the accuracy of shrinkage compensation mechanisms [71]. 4.4. Milling Scale Subclassification: Micro Milling Technology 4.4.1. Burs Dependent Micromilling Microscopically detailed milling is feasible using cutting tools as small as 0.1 mm, and even smaller tools might be available for special object production [72]. Very fine microscopic details have been able to be carved on the surfaces of PEEK material using 0.0167–0.025 mm and 0.05–0.15 mm cutting tips, the surface finish of the produced part depends on the milling process used [73]. This high-tech micro-milling might be suitable for producing featured dental parts like implant fixtures and screws [74]. Nevertheless, this process is also not efficient in producing hollow and complex structures, even if it could produce the desired surface’s fine details. Besides that, it will be very costly; the cutting tools are rapidly worn by cutting certain materials as PEEK. The known main application of micro-milling found its benefit in the characterizations of additively manufactured objects [75], the combination of the latter two technologies might raise production in dentistry to the next level. The micromilling is applied mostly to produce industrial metal parts, with the diameter of the tools ranging between 100–300 µm. The smallest cutting tools applied in dentistry come with a 0.3 mm diameter or larger as shown in Figure 8. Smaller, high-tech milling dimensions are available for ultimate precision. However, these advanced technologies may not be strongly indicated for dental purposes, as micrometer- and nanometer-scale surfaces and structures are not yet applied in the dental field. However, in the medical field, they are true of great advantage, used for high-tech complex and intricate Nanoscale drug delivery systems [76], microneedles [77], and titanium bone implants with surface roughness made by micromilling to induce osseointegration [78]. The latter application might benefit implant dentistry, featuring implant surfaces, creating precise custom-made connections, and improving overall efficiency. 4.4.2. Laser Micromachinery Laser technology has been applied in various medical and dental fields, including healing, surgical procedures, machinery, and production. In this section, lasers were discussed in terms of micromilling and their applications in the dental and medical fields. 4.4.2.1. Laser Micromilling and Surface Featuring Precise and efficient micromachinery was achieved using laser, with half-micron surface roughness, and high accuracy and precision matching the original CAD model. This technology proved successful for medical device applications, such as lithium-anobate-based resonant sensors [79]. The production of biodegradable stents for peripheral blood vessels with 100 µm diameter was feasible and practical [80]. Moreover, the laser is capable of sub-5 µm featuring, and 1.5 µm shadow masks [81]. Laser micromachinery is used primarily in dentistry to feature dental implant surfaces, as a key method for enhancing osseointegration, cellular proliferation, and antibacterial potential, contributing significantly to implant success and longevity. Research on laser-modified titanium surfaces has demonstrated its ability to influence various biological and mechanical aspects of dental implantology. Laser treatment plays a pivotal role in enhancing osseointegration, the process by which the implant integrates with bone. Multiple studies have shown that laser-modified surfaces improve the biomechanical stability of implants. For instance, Faeda et al. [82] demonstrated that Nd: YAG laser-modified titanium implants exhibited significantly higher removal torque (RTQ) values over various healing periods, reflecting enhanced bone-to-implant contact and stability over time. Other research, such as that by Hallgren et al., revealed that laser-treated implants, which feature grid-like pits, increased interfacial surface area and retention forces, potentially promoting better osseointegration compared to untreated surfaces [83]. A hydrophilic surface tends to enhance initial cell adhesion, proliferation, and bone mineralization, resulting in improved osseointegration compared to hydrophobic surfaces [84]. Research indicates that laser-textured surfaces with specific patterns, such as micro-grooves or pits, can improve bone-to-implant contact (BIC) by facilitating directional cell alignment and migration. These topographical modifications are crucial for enhancing implant stability and bone formation [85]. Laser-modified implant surfaces show a positive influence on osteoblast vitality, adhesion, and proliferation. In particular, laser-induced modifications can create surface textures that enhance the attachment of bone-forming cells. Györgyey et al., conducted in vitro studies and concluded that despite some damage to titanium oxide layers, the modified surfaces promoted robust osteoblast cell proliferation [86]. Additionally, studies by Zwahr et al. reported an increase in osteoblast vitality and wettability on laser-modified titanium surfaces, which are critical factors in facilitating cellular attachment and proliferation [87]. Laser surface texturing influences cellular responses at the tissue-implant interface. Regular patterns created through laser treatment encourage the alignment, migration, and proliferation of cells [88]. For instance, mesenchymal stem cells cultured on laser-textured surfaces align along the groove direction, which enhances osteogenic differentiation and metabolic activity. This accelerates bone formation and reduces implant healing time [89]. Moreover, laser-treated implants with micro-grooves increase BIC and improve overall biological responses compared to non-textured implants [90]. Laser-modified surfaces also exhibit antibacterial properties, which help reduce peri-implantitis—a leading cause of implant failure due to bacterial inflammation. Cunha et al., demonstrated that laser-modified titanium surfaces reduced bacterial adhesion and biofilm formation, specifically against Staphylococcus aureus, one of the primary pathogens responsible for peri-implantitis. The study showed that surface textures created by the laser, such as nano-spikes, played a significant role in preventing bacterial colonization [91]. Superhydrophobic and superhydrophilic surfaces created by laser processing are effective in reducing biofilm formation on implant surfaces [92]. Additionally, Laser-Induced Periodic Surface Structures (LIPSS), which have feature sizes smaller than bacteria, can further reduce bacterial adhesion and biofilm formation [93]. Combining laser surface texturing with antibacterial coatings, such as gold and silver nanoparticles, has also been explored as a strategy to enhance the antibacterial properties of implants [94]. Laser treatments can also improve force distribution in dental implants, as shown by Celen and Özden [95]. By creating specific surface patterns like honeycombs, lasers can mimic natural periodontal ligament structures, thus enhancing force transmission and potentially reducing bone resorption [95]. Furthermore, a study by Man et al. demonstrated that surface textures generated by laser irradiation improved nutrient circulation, which could lead to the deeper migration of bone cells and better implant retention [96]. 4.4.2.2. Role in Ceramic Adhesion and Veneering Several research and trials have been conducted to improve the adhesion potentials of prosthetic and restorative parts. Development is continuing in adhesive luting agents and their corresponding bonding agents and primers. Other aspects of adhesion represented by surface treatment of the substrates are pivotal in utilizing strong, reliable, and durable adhesion, particularly for surface treatment of chemically inert materials, such as zirconia [37]. Metal and metal alloys were acid-etched or tin-plated in vintage adhesion protocols. Nowadays, metal surfaces are treated by air-particle abrasion using mostly AL2O3 particles with different dimensions and air pressure. Glass-ceramic materials, such as lithium disilicate, are etched with a suitable acid-etchant—5% hydrofluoric acid for 20 seconds [97]. In contrast, high-strength oxide ceramics, such as zirconia, are chemically inert and are treated using air particle abrasion (APA) or silica coating [98]. Although adhesion potential increased with phosphate monomer-containing adhesives [37], micromechanical retentive means utilized from surface roughness is the standard step in which all the adhesive protocol success is built. To increase surface roughness without destroying the microstructure of the part intended for adhesion, laser micromilling of intaglio surfaces is recommended. This is done by creating microgrooves and wafer forms on the restorative and prosthetic parts, aiming to enhance their resistance to debonding [99]. Moreover, the laser surface texturing was applied to lithium disilicate ceramic and could enhance adhesion reliability and durability [99,100]. A femtosecond laser was able to create very fine microgrooves with 2.5 µm diameter [101], Figure 9 Given that air particle abrasion is not recommended for lithium disilicate ceramics, laser surface texturing might be a viable substitute for HF acid etching [102]. Laser micromilling of zirconia surface results in well-oriented and designed micro features, with increased wettability and adhesion potential and no signs of microcracks or structural changes [100]. Clinical application of laser micromilling is not recommended due to the high hazard of the technology. Besides, repair of broken zirconia core and ceramic veneering restorations revealed no significant enhancement of repair bond [103]. Confirming that these costly and hazardous devices are better installed in dental labor and manipulated by highly professional and skilled practitioners to avoid any risky complications.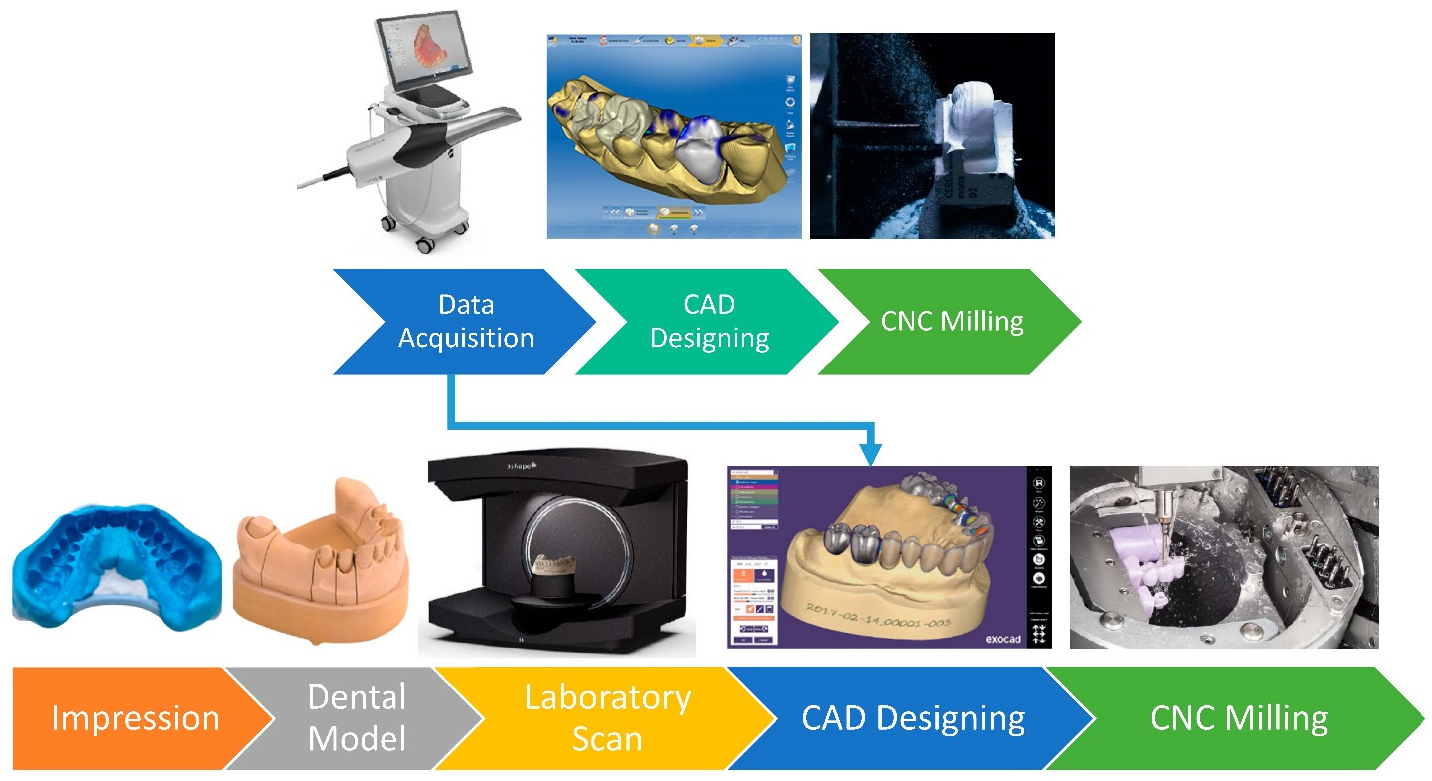
Main System and Model
Company and Country of Origin and Release Date
CAM Driving Software
View of the Machine
Milling Burs
Milling Speed and Time for a Single Crown
Fabrication Materials
Main Features
Drawbacks
Research Findings
CEREC 3
Sirona Germany
2000CEREC SW

2 stepping motors
Step Bur 10
Step bur 12
Cylinder Pointed Bur Cylinder Bur 1.2 mm Cylinder Bur 1.6 mm40.000 rpm
Feldspathic ceramic blocks, specifically Vita Mark II.
4-axis milling, both wet and dry milling, complete chairside system, high precision
Limited to specific ceramic blocks (Vita Mark II), potentially limiting material options
CEREC 3 reliably produces dental restorations with a good marginal fit [22].
Crowns maintain good accuracy with a luting space set at 30 µm [23].
CEREC MC X Mill
Sirona Germany
2007CEREC SW

Step Bur 12 and 12S
Cylinder Pointed Bur 12S and 12 EF
Step Bur 20
Cylinder Pointed Bur 20
Shaper 25 RZ
Finisher 10
Shaper 25approximately 10 minutes
Feldspar ceramic, Glass-ceramics, Full contour zirconia, Hybrid ceramic, Polymer blocks
4-axis milling
Complete digital workflow
Precise and fast, can take 10 minutes for a single crown
Can produce a surgical guide
It can be used in lab.The limited block size for chairside treatment. Restricted to 40 millimeters
The study found similar margin accuracy for both CEREC 3 and CEREC MC X Mill machines [22].
CEREC Primemill
Sirona Germany
2019CEREC Software 5

Bur 2.5 ZrO2 CS
Bur 2.5 PMMA CS
Bur 1.0 CS
Bur 0.5 CSabout five minutes
Zirconia, glass, and hybrid ceramics
4- axis milling
Multiple speeds, including superfast milling, finishing zirconia crown in less than 5 minutes.
It can mill a wide variety of materials.Very expensive
Provides only dry milling
Limited to simple restorations and prostheses.Superfast, fast, and fine milling all produce surface roughness within the acceptable range [20].
Planmeca Planmill 30s one spindle
Planmeca Oy.
Finland
2017Planmeca Romexis® software

Diamond Grinders
(tapered, conical, ellipsoidal)100,000 RPM
16 to 18 min/crownGlass-ceramics, hybrid materials, zirconia
single-spindle milling unit designed for wet milling. Offering affordability, precision, and ease of use for dental practices.
Limited to wet processing only
Demonstrated a marginal discrepancy averaging 85–96 microns, suggesting good accuracy for ceramic restorations [24].
Planmeca Planmill 40s two spindles
Planmeca Oy.
Finland
2020PlanCAD Easy

Diamond Grinders
(tapered, conical, ellipsoidal)100,000 RPM
10 min/crownCeramics, Hybrid Ceramics, Zirconia, and Resin-Based Materials
5-axis, wet and dry milling, automatic changer for 12 tools, integrated PC with touchscreen, Open platform for importing and editing files
Relatively high weight (160 lbs).
The Planmeca PlanMill 40S offers higher accuracy compared to the PlanMill 30S model [24].
Planmeca
PlanMill 35 Milling UnitPlanmeca Oy.
Finland
2023Planmeca PlanCAD

CUTTER 1 MM BALL END
Grinder ellipsoidal tip RTI 4 mm shank100,000 rpm/
11–13 minutesGlass-ceramicPMMACompositeHybrid ceramicZirconia
4-axis, wet and dry milling, high precision, future-proof investment, easy operation Compatible with various parties
Require additional setup for dry milling capabilities
Carestream Dental
CS 3000Carestream Dental
United States, 2013Carestream Dental imaging software

Single bur milling
Four-axis brushless motorUp to 60,000 RPM
15 min/crownVITABLOCS Mark II
4-axis milling, wet milling, complete chairside system for single-unit restorations
Limited milling capabilities (single-unit restorations only), may require a separate acquisition unit
Carestream Dental
CS 3100Carestream Dental
United States, 2019exocad ChairsideCAD software

Up to 100,000 rpm/Less than an hour.
Hybrid resin, ceramic, and zirconia.
A self-contained 4-axis wet milling with CAD software; Suited for crowns, bridges, inlays, onlays, and veneers; Smart Milling Queue Management
The system may have limited compatibility with certain CAD software or scanners.
Chairman from Robots and Design
MAXX SeriesRobots and Design,
South Korea, 2021Go2CAM

Shank diameter: 3 mm, ATC 6 tools
3 tools for left spindles and 3 tools for right spindles100,000 RPM, 8 to 15 minutes
Glass-ceramic (Lithium Silicate, Lithium Disilicate), Zirconia, PMMA, Hybrid ceramic
3-axis with dual spindles, integrated with Exocad, and featuring remote operation via MAXXLink, streamlines workflow effortlessly. Produce ultra-thin veneers (0.3 mm or less)
The lack of automatic material-changing functionality means that users must manually switch materials
Versamill the chairmaxx
From Axsys Dental SolutionAxsys Dental Solution, USA, 2023
Open system

Shank diameter: 3 mm, ATC 6 tools
3 tools for left spindles and 3 tools for right spindles100,000 rpm, 8–15 minutes
glass-ceramic, hybrid-ceramic, zirconia, and PMMA.
5-axis, easy, high accuracy (precision up to less than 20 micrometers)
Open system, compact, and quiet designLimited to wet milling only
Glidewell Laboratories
IOS TS150 Chairside MillGlidewell Laboratories, USA, 2013
Open system

BUR WRENCH 11 mm X 9 mm–3 mm shank
150,000 RPM, 20 minutes
Obsidian™ Lithium Silicate Ceramic, BruxZir® Solid Zirconia
Open-system, for glass ceramic crowns, resin nano ceramic, and PMMA materials.
Primarily for crowns, limiting its versatility.
Dynamic Chairside milling machine
Dynamic Medical Technology, China, 2023

Three models included: 0.5 mm, 1.0 mm, 2.0 mm.
Up to 60,000 rpm /
Zirconia, PMMA, Wax, Hybrid, feldspathic and glass ceramics, etc.
Five-axis wet and dry milling, high-precision spindle, large angle cutting, compact design, flexible and efficient cutting, thickness down to 0.3mm for ultra-thin veneer.
Air compressor required (minimum air pressure 0.45 Mpa), limited to three bur sizes.
![Figure 7: <p>(<strong>A</strong>). The axis of movements of the spindle and holding base for the 5-axis milling machine. (<strong>B</strong>). The 6-axis milling machines contain extra vertical movement of the base (blue arrow at the H plane). (<strong>C</strong>). Links reference systems and parameters of 5-axis milling machines. (<strong>D</strong>). Links reference systems and parameters of the 6-axis milling machines [<a href="#ref56">56</a>].</p>](/uploads/source/articles/biomaterials-connect/2025/volume2/20250013/image007.png)
![Figure 9: <p>Laser micromachinery; macroscopic and microscopic images of the grooves and ridges created on the surface of zirconia disc [<a href="#ref101">101</a>].</p>](/uploads/source/articles/biomaterials-connect/2025/volume2/20250013/image009.png)
5.1. Intracoronal Restorations and Fixed Dental Prostheses In the realm of indirect restorations, the main procedure predominantly involves chairside milling of glass ceramic and composite resin blocks [34]. The idea of milling restorations from blocks was first applied by Dr. Mörmann, with the requirement of decent hardness for machinability and good quality for restoration and tool integrity after the milling process. Feldspathic ceramic blocks (Vita Zahnfabrik) were first adopted [17]. The development of the technology led to the adoption of more metal and ceramic materials, such as lithium disilicate glass-ceramic [104]. Moreover, it led to the development of only digital manufacturing materials, such as zirconia and alumina oxide ceramics, zirconia-reinforced lithia silicate [104,105], and polymer-infiltrated ceramic network (PICN) [106]. In terms of restoration design and geometric complexity, inlays and onlays present more intricate designs compared to crowns [34]. This plays a pivotal role in discerning the disparities in adaptation [45,47,107,108]. The type of milling device utilized can influence the outcome of adaptation, especially for restorations with intricate shapes, deep grooves, and internal angles [11,33,43,44,45,48,109]. For over two decades, CAD/CAM technology has revolutionized esthetic dentistry, transforming diagnosis, planning, and treatment. Thanks to technology, the resin-bonded bridges utilize zirconia and alumina esthetic wings instead of the traditional veneered metal prostheses, with very high clinical survival, reaching 95% after 15 years in the case of zirconia [38], reflecting the excellent physical-mechanical properties of zirconia restorations and their reliable bonding potential [37]. In the context of milled veneers, the use of CAD/CAM technology has been documented to deliver exceptional precision and operational efficiency [110]. Likewise, the CAD/CAM technology succeeded in producing thin and ultrathin occlusal veneers with thicknesses ranging from 0.3–0.5 mm, utilizing a wide variety of materials and investigated for both clinical and laboratory records [111,112]. The fabrication of ultrathin restorations with a minimum of 0.1 mm thickness was feasible, PICN non-prep technique full mouth rehabilitation of wear dentition showed promising results. However, the very thin margins were more prone to chipping at the posterior region of the mouth, particularly in occlusal risk factors [111,113]. A new design of posterior cantilever prostheses with thin occlusal veneer retainer was feasible, the restorations survived the clinical simulation and possess a durable adhesion with an excellent debonding resistance [37]. Furthermore, the CAD/CAM production of special design zirconia attachment showed clinically high esthetic outcomes compared with the traditional attachment systems [114]. With all these capabilities, challenges always facing CNC milling procedures, such as chipping of thin margins or fracture of constricted areas [68], discrepancies in the incisal overlap, labial or occlusal surfaces of occlusal and laminate veneer restorations, which are better overcome by the rising 3D printing technology [2,5]. In terms of full coverage restorations, metal crowns made through traditional casting, 3D printing, and CNC milling revealed clinically acceptable margins within 120 μm [16,115]. However, CNC milling might offer superior internal and marginal fit compared to the conventional method [16], and better marginal fit compared with 3D printing [2]. The 5-axis Kavo Everest milling system produced a titanium crown with a 60–80 μm vertical gap, significantly higher than the cast noble metal crowns [116,117]. Nevertheless, the conventional technique marginal gap is relevant depending on the skills of the technician, while CAD/CAM is more standardized and less influenced by human-induced errors [2,5]. The duration of the milling process is primarily determined by the tool path, which is influenced by cutting parameters such as the step-over distance, feed rate, spindle speed, and cutting depth [118]. The modern advanced machines have paved the way for high-speed milling, finishing a single dental crown in less than 5 minutes [20]. For milled composite resin crowns, the surface smoothness can be enhanced by reducing the step-over distance; however, this adjustment tends to increase the processing time [118]. Despite the varying cutting conditions, the flexural strength of milled composite resin remains within clinically acceptable limits, even under the roughest conditions. Nonetheless, it’s important to avoid milling conditions that make the surface rougher than a sandblasted finish, as this might compromise the flexural strength of the material [118]. This was evident in the modern CEREC chairside Primemill, the ultrafast milling produced crown with a rougher surface than fine milling, however, all the speed options; Super-Fast/Good, Super-Fast/Very Good, Fast, and Fine; produce zirconia crown within the expected range of surface roughness [20], see Supplementary Table S1, available online. According to a study by Lüchtenborg et al., subtractive manufacturing of zirconia FDPs was more accurate than 3D printed FDPs, with mean deviations smaller than 50 μm in all areas, aligning with previous reports of marginal discrepancies ranging from 17 to 118 μm for milled zirconia bridges [119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135]. These results emphasize the exceptional quality of subtractively manufactured FDPs [134]. Subtractive manufacturing relies on pre-made blanks to guarantee uniform powder compaction, manageable shrinkage, and precise predictability of dimensional alterations during sintering. Conversely, the homogeneity of the 3D-printed green body can be disrupted, for example, by its layered structure, leading to anisotropic shrinkage during sintering [136,137]. This has the potential to detrimentally impact the predictability and ultimate precision of 3D-printed components [134]. 5.2. Implant Fixture, Abutments, and Superstructure The integration of CAD/CAM technology in milling implant fixtures has revolutionized dental implantology, enhancing accuracy, robustness, and aesthetic quality [138]. These fixtures, made from biocompatible materials such as pure titanium, titanium alloys, and high-grade ceramics like alumina and zirconia, are essential for supporting prosthetic elements attached to the bone [139]. The CAD/CAM system generates a digital blueprint of the required fixture using advanced software, which the milling machines use to carve the implant from a solid material block with exceptional precision. This accuracy is essential for ensuring the implant fits seamlessly into the jawbone, minimizing the risk of failure due to improper fitting [140,141]. The system’s ability to process various materials allows for individualized dental implant practices. Moreover, precise surface treatments applied during milling enhance osseointegration, which is crucial for the implant’s long-term viability and stability [141,142]. This cleared the way for improving surface characterization by laser treatment, surface coatings, or 3D bioprinting to CNC milled implant fixtures, which further enhanced the biological reaction of tissues, osteoinduction, and osseointegration of dental implants, contributing significantly to long-term survival [143]. Custom abutments are mainly made from titanium or zirconia ceramic and less commonly from lithium disilicate, polymer-infiltrated ceramics, and PEEK. Milled titanium and zirconia abutments exhibit vertical gaps of 2.5–3.2 μm and minimal rotational movement [144,145]. Milling consistently produces highly accurate implant frameworks with a vertical fit of 1 to 27 μm [13], unaffected by the prosthesis span, unlike cast metal frameworks [36,146,147]. Milled abutments also have minimal surface roughness, precise geometric edges, and a vertical gap of 0.7 μm, outperforming selective laser melting (11.3 μm) and casting (9.1 μm) methods [148]. CAD/CAM milled Co-Cr bars possess superior internal fit at the implant-abutment interface compared to those made by selective laser melting (SLM) 3D printing or traditional lost wax techniques [149,150,151]. 5.3. Resins and Waxes for the Conventional Lost Wax Method Traditionally, handcrafted natural wax patterns have been the norm, requiring highly skilled technicians and precise building of the pattern but prone to human-related errors affecting the accuracy of the fabricated crowns [152,153,154]. For standardization of the produced resin and wax patterns, the production of wax patterns has transitioned to various CAD/CAM methods [152]. These include subtractive methods like milling and additive manufacturing, which have effectively mitigated many limitations inherent in conventional waxing techniques [155]. Crowns and inlays cast from milled wax patterns showed higher accuracy of fit than crowns and inlays cast from manually built patterns [156,157]. However, this is relevant to the skills of the technician building the wax and the type of restoration or prostheses, as simple heat-pressed ceramic restorations might produce comparable accuracy [158] or higher trueness than milled restorations [159]. 5.4. Models’ Fabrication Optical impressions have gained greater prominence, necessitating new methods for model fabrication. As alternatives to poured stone casts, including milling and 3D printing of dental models [160,161,162,163]. Yau et al. demonstrated that the accuracy of dental models manufactured through milling surpassed those produced by 3D printing [162]. The decreased precision observed in 3D printed models was ascribed to the staircase effect on the surfaces formed through layer-by-layer deposition and model distortion stemming from polymerization shrinkage [160,163]. Conversely, a study demonstrated that the accuracy of milled and 3D-printed PMMA working models showed similarities [164]. 5.5. Removable Partial and Complete Dentures The fabrication of removable partial denture (RPD) frameworks has seen a shift toward using resin-based polymers, replacing the traditional cobalt chromium. These innovative polymers are typically produced in puck or disc forms and are subjected to milling processes to create the final denture frameworks [165]. A significant advantage of these materials is that they generally require minimal post-milling adjustments, finishing, and polishing [165]. Milling metal frameworks for RPDs, particularly from cobalt chromium or titanium blocks, presents technical challenges, mainly due to the significant wear and tear on milling burs, especially with base metals [166]. The metal frameworks could be produced indirectly by casting milled wax or resin-milled patterns or directly by milling the frameworks from metal alloy discs. Additionally, the denture base and teeth can be milled from corresponding prefabricated discs and subsequently assembled using adhesive binding (Figure 10). The term “milled Co-Cr/Ti framework” sometimes refers to resin or wax patterns milled from wax or resin discs and then cast traditionally [165]. Numerous records compared the fitting accuracy of frameworks created from 3D-printed and milled resin patterns to those made through traditional casting techniques. The results vary from one record to another. However, all three methods produce frameworks within clinically acceptable tolerances [168,169,170,171,172]. Efforts to mill frameworks using titanium discs face challenges due to titanium’s difficult machinability compared with other alloys, resulting in prolonged producing times and increased wear of cutting tools [173,174]. This wear reduces milling accuracy and increases material waste, making titanium milling inefficient [165]. Before incorporating CAD/CAM technology into removable prosthodontics, achieving perfect alignment between the denture base and denture-bearing tissues was challenging due to the polymerization shrinkage of the resin [175]. This shrinkage often caused distortions in the denture base, negatively affecting the fit and retention of complete removable dentures [176,177,178]. Subtractive manufacturing, which uses dense prefabricated polymethyl methacrylate (PMMA) discs pre-polymerized under high-temperature and high-pressure conditions, eliminates this issue. As a result, the final CNC-machined prosthesis does not undergo polymerization during manufacturing [179,180,181], Figure 11. However, this method faces challenges in accessing undercut areas due to the limitations of milling bur size and milling axes [180,181,182]. Research shows that complete removable dentures produced through CAD/CAM milling methods exhibit superior retention, accuracy, and mechanical characteristics while eliminating polymerization issues compared to conventional or injection-molded dentures [183,184,185,186]. The CAD/CAM monolithic (fully-milled) processing technique demonstrated the highest accuracy in tooth movements, followed by fluid resin, CAD-CAM-bonded, pack-and-press, and injection molding [187]. Additionally, milled complete dentures may reduce the occurrence of Candida-associated denture stomatitis over time [188,189].![Figure 10: <p>RPD fabricated by digital workflow with milling technology, A and B CAD virtual designing, (<strong>A</strong>) Offsetting metal framework, (<strong>B</strong>) Combining the offset metal framework and denture base, (<strong>C</strong>) Metal framework seated on stone cast, (<strong>D</strong>) Milled denture base and offset metal structure complex, (<strong>E</strong>) Completed removable partial denture [<a href="#ref167">167</a>].</p>](/uploads/source/articles/biomaterials-connect/2025/volume2/20250013/image010.png)
![Figure 11: <p>Directly milled complete denture, (<strong>A</strong>) Milled denture base, (<strong>B</strong>) Milled denture teeth, (<strong>C</strong>) The finished denture base and teeth for maxillary complete denture [<a href="#ref190">190</a>].</p>](/uploads/source/articles/biomaterials-connect/2025/volume2/20250013/image011.png)
Subtractive manufacturing faces several limitations. Firstly, the initial investment and the production costs for the CNC milling system are quite high [191]. By CNC milling of the discs or blocks, the greater mass of the prefabricated raw material is wasted, resulting in excessive material consumption [192,193], making it challenging to repurpose the discarded material [194]. This waste represents both an economic and environmental concern [194]. The cutting tools are subjected to continuous wear and damage, they can be used only for limited cutting cycles, implying their constant replacement, as they can be used only for limited milling cycles [195]. The CNC milling possesses some inherited limitations in the milling of dental parts with complex geometry or hollow structures. As the fabrication of hollow structures is impossible using milling technology, the fabrication of intricate dental parts is very time-consuming, as the computer numerically controlled (CNC) unit is highly constrained to angulations [196], which restricts access to small hollow areas bypassing the undercuts [192]. Additionally, there are limitations imposed by drill accessibility, particularly for sharp interior angles [197]. Moreover, the milling accuracy depends on the size of the cutting tool and the number of milling axes of the CNC machine [195]. In these scenarios, the milling machine employs “drill compensation” to remove material that should be cut away, which, in the context of a dental crown, means that more material is removed than intended [197]. This can result in areas with a thicker layer of cement material than desired [197]. Furthermore, the grinding of certain materials, such as dental ceramic blocks or discs, can generate micro-cracks within the internal structures [198], and the grinding of polymeric materials such as PEEK is challenging. Polymeric materials require special handling to reduce heat-related cracks and internal stresses; annealing is necessary for such materials; the polymers do not dissipate heat well compared with other materials, such as metal; by deep drilling, the produced parts can crack. Regardless of all these drawbacks, CNC milling has been used successfully in the dental field for the last four decades, producing several dental parts, from dental restorations to implant fixtures and superstructures and complete arch frameworks. CNC milling nowadays is the first production technology in the dental field. These mentioned drawbacks emphasize that there will always be room for further investment and development of the technology and their driving software. It is not known yet if the utilization of more than 5-axis milling machines could improve the efficiency and speed of milling. Moreover, the utilization of lath parts in the machine could be advantageous in the fabrication of inner structures such as the screw housing of dental implant fixtures. Highly specified CNC devices are not yet utilized in the dental field, such as micromilling devices, which can produce very refined and detailed features of the surface. Combining milling technology and additive manufacturing might improve hybridization in dentistry, for example, the fabrication of hybrid root analog dental implants [199]. Moreover, future ideas such as the characterization of surfaces, surface coating of milled parts with antibacterial bioactive materials [200], or building intricate hollow structures within or over large simple geometrical milled parts [201]. Within the domain of intelligent manufacturing, there is a growing emphasis on intelligent milling, particularly in the context of online monitoring and milling parameters optimization [202,203]. The monitoring of milling conditions, encompassing aspects such as tool wear condition, chatter, and vibration relative to machine stability, is emerging as a pivotal research domain in the realm of intelligent digitization and subtractive manufacturing [204]. Moreover, the tool wear prediction is garnering increased attention to enhance part quality by minimizing attrition rates, ultimately enhancing production efficiency and manufacturing sustainability [205].
CNC milling has been successfully used in the dental field for several decades and is currently the main production technology. Some dental devices, such as orthodontic appliances, occlusal splints, surgical guides, and dental models, have been preferably produced by additive manufacturing, but in restorative and prosthetic dentistry, for chairside and laboratory production, CNC milling is the predominant and most preferable method up to date. Although CNC-milled restorations, prostheses, and other dental parts are reported to be successful, there is still room for further investment and development to address limitations such as material waste, time-consuming fabrication of complex dental parts, and accuracy issues. Moreover, the adoption of advanced milling machines with more than 5 axes, incorporating lathe parts, and integrating additive manufacturing techniques can potentially enhance efficiency, speed, and the fabrication of intricate structures in dentistry. Additionally, intelligent manufacturing focuses on online monitoring, optimizing milling parameters, and predicting tool wear to improve part quality, minimize scrap rates, and enhance the sustainability of manufacturing processes.
3D
Three Dimensional
AL2O3
Aluminium Oxide
APA
Air-Borne Particle Abrasion
BIC
Bone-to-Implant Contact
CAD
Computer-Aided Design
CAM
Computer-Aided Manufacturing
CEREC
CERamic REConstruction or Chair-side Economical Restoration of Esthetic Ceramic
CNC
Computer Numerical Control
Co-Cr
Cobalt-Chromium
Co-Cr/Ti
Cobalt-Chromium/Titanium
FDPs
Fixed Dental Prostheses
LIPSS
Laser-Induced Periodic Surface Structures
NC
Numerical Control
PEEK
Polyetheretherketone
PMMA
Polymethyl Methacrylate
RPD
Removable Partial Denture
SLM
Selective Laser Melting
M.A.A. Conceptualization, project administration, validation, visualization, writing and reviewing the primary draft, writing and reviewing the main manuscript, and supervision. R.A., S.A., and W.A. Data collection, methods, data curation, writing the primary draft, visualization. A.Y.A. Conceptualization, validation, writing and reviewing the main manuscript, supervision.
The authors confirm that all human images included in this manuscript were used with proper consent obtained from the individuals depicted, permitting their publication in this article.
The authors declare no conflicts of interest in the companies or products used in this study.
This review received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The authors would like to thank the Institute of Digital Dentistry, particularly Ahmad Al-Hassiny (https://instituteofdigitaldentistry.com/) for allowing us to use some images from their website to enhance the visualization of this comprehensive review.
Table S1 and Table S2 are available here.
[1] Schierz, O.; Hirsch, C.; Krey, K.-F.; Ganss, C.; KÄMmerer, P.W.; Schlenz, M.A. Digital dentistry and its impact on oral health-related quality of life. J. Evid.-Based Dent. Pract. 2023, 24, 101946. [CrossRef] [PubMed]
[2] Alghauli, M.; Alqutaibi, A.Y.; Wille, S.; Kern, M. 3D-printed versus conventionally milled zirconia for dental clinical applications: Trueness, precision, accuracy, biological and esthetic aspects. J. Dent. 2024, 144, 104925. [CrossRef] [PubMed]
[3] Bertelè, M.; Minniti, P.P.; Dalessandri, D.; Bonetti, S.; Visconti, L.; Paganelli, C. A computer-guided minimally-invasive technique for orthodontic forced eruption of impacted canines. Minerva Stomatol. 2016, 65, 176–184. [PubMed]
[4] ElAskary, A.; Elfana, A.; Meabed, M.; Abd-ElWahab Radi, I.; Akram, M.; Fawzy El-Sayed, K. Immediate implant placement utilizing vestibular socket therapy versus early implant placement with contour augmentation for rehabilitation of compromised extraction sockets in the esthetic zone: A randomized controlled clinical trial. Clin. Implant. Dent. Relat. Res. 2022, 24, 559–568. [CrossRef] [PubMed]
[5] Alghauli, M.A.; Alqutaibi, A.Y. 3D-printed intracoronal restorations, occlusal and laminate veneers: Clinical relevance, properties, and behavior compared to milled restorations; a systematic review and meta-analysis. J. Esthet. Restor. Dent. 2024, 36, 1153–1170. [CrossRef] [PubMed]
[6] Yousry, M.; Hammad, I.; El Halawani, M.; Aboushelib, M. Preparation of ultrathin translucent zirconia laminate veneers using 3D printing reduction guides. J. Prosthet. Dent. 2024, 131, 548–553. [CrossRef]
[7] de Oliveira, D.; Souza, F.I.; Caixeta, M.T.; Duque, C.; Oliveira, S.H.P.; Rocha, E.P. Clinical and Microbiologic Outcomes of Ceramic Laminate Veneers Bonded to Teeth Without a Finish Line: 1-year Results of a Prospective Study. Int. J. Prosthodont. 2023, 36, 244–252. [CrossRef]
[8] Mangano, A.; Beretta, M.; Luongo, G.; Mangano, C.; Mangano, F. Conventional Vs Digital Impressions: Acceptability, Treatment Comfort and Stress Among Young Orthodontic Patients. Open Dent. J. 2018, 12, 118–124. [CrossRef]
[9] Chainani, P.; Paul, P.; Shivlani, V. Recent Advances in Orthodontic Archwires: A Review. Cureus 2023, 15, e47633. [CrossRef]
[10] Alqutaibi, A.Y.; Hamadallah, H.H.; Alturki, K.N.; Aljuhani, F.M.; Aloufi, A.M.; Alghauli, M.A. Practical applications of robots in prosthodontics for tooth preparation and denture tooth arrangement: A scoping review. J. Prosthet. Dent. 2024, . [CrossRef]
[11] Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 60, 72–84. [CrossRef] [PubMed]
[12] Rekow, E.D.; Silva, N.R.; Coelho, P.G.; Zhang, Y.; Guess, P.; Thompson, V.P. Performance of dental ceramics: Challenges for improvements. J. Dent. Res. 2011, 90, 937–952. [CrossRef] [PubMed]
[13] Abduo, J.; Lyons, K.; Bennamoun, M. Trends in computer-aided manufacturing in prosthodontics: A review of the available streams. Int. J. Dent. 2014, 2014, 783948. [CrossRef]
[14] Rekow, E.D.; Erdman, A.G.; Riley, D.R.; Klamecki, B. CAD/CAM for dental restorations--some of the curious challenges. IEEE Trans. Biomed. Eng. 1991, 38, 314–318. [CrossRef] [PubMed]
[15] François, D. . The Optical Impression ; University Claude-Bernard: Lyon, France, 1973; . .
[16] Chou, W.T.; Chuang, C.C.; Wang, Y.B.; Chiu, H.C. Comparison of the internal fit of metal crowns fabricated by traditional casting, computer numerical control milling, and three-dimensional printing. PLoS ONE 2021, 16. [CrossRef]
[17] Mörmann, W.H. The evolution of the CEREC system. J. Am. Dent. Assoc. 2006, 137, 7s–13s. [CrossRef] [PubMed]
[18] Mörmann, W.H.; Brandestini, M.; Lutz, F. The Cerec system: Computer-assisted preparation of direct ceramic inlays in 1 setting. Quintessenz 1987, 38, 457–470. [PubMed]
[19] Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [CrossRef]
[20] Fasbinder, D.J.; Duddanahalli Siddanna, G. Surface Evaluation of Milled Chairside CAD/CAM Materials Based on Manufacturing Speed. Int. J. Comput. Dent. 2023, . [CrossRef]
[21] Blatz, M.B.; Conejo, J. The Current State of Chairside Digital Dentistry and Materials. Dent. Clin. N. Am. 2019, 63, 175–197. [CrossRef]
[22] Roperto, R.; Assaf, H.; Soares-Porto, T.; Lang, L.; Teich, S. Are different generations of CAD/CAM milling machines capable to produce restorations with similar quality?. J. Clin. Exp. Dent. 2016, 8, e423–e428. [CrossRef]
[23] Nakamura, T.; Dei, N.; Kojima, T.; Wakabayashi, K. Marginal and internal fit of Cerec 3 CAD/CAM all-ceramic crowns. Int. J. Prosthodont. 2003, 16, 244–248. [PubMed]
[24] Vag, J.; Nagy, Z.; Bocklet, C.; Kiss, T.; Nagy, A.; Simon, B.; Mikolicz, A.; Renne, W. Marginal and internal fit of full ceramic crowns milled using CADCAM systems on cadaver full arch scans. BMC Oral. Health 2020, 20. [CrossRef] [PubMed]
[25] Kurbad, A. Cerec goes inLab--the metamorphosis of the system. Int. J. Comput. Dent. 2001, 4, 125–143. [PubMed]
[26] Zuercher, A.N.; Ioannidis, A.; Hüsler, J.; Mehl, A.; Hämmerle, C.H.F.; Thoma, D.S. Randomized controlled pilot study assessing efficacy, efficiency, and patient-reported outcomes measures of chairside and labside single-tooth restorations. J. Esthet. Restor. Dent. 2023, 35, 74–83. [CrossRef]
[27] Hanoon, Z.A.; Abdullah, H.A.; Al-Ibraheemi, Z.A.; Alamoush, R.A.; Sami, S.M.; Haider, J. Marginal Fit of Porcelain Laminate Veneer Materials under Thermocycling Condition: An In-Vitro Study. Dent. J. 2023, 11. [CrossRef]
[28] Kanazawa, M.; Inokoshi, M.; Minakuchi, S.; Ohbayashi, N. Trial of a CAD/CAM system for fabricating complete dentures. Dent. Mater. J. 2011, 30, 93–96. [CrossRef] [PubMed]
[29] Yoon, S.N.; Oh, K.C.; Lee, S.J.; Han, J.S.; Yoon, H.I. Tissue surface adaptation of CAD-CAM maxillary and mandibular complete denture bases manufactured by digital light processing: A clinical study. J. Prosthet. Dent. 2020, 124, 682–689. [CrossRef] [PubMed]
[30] Pilecco, R.O.; Machry, R.V.; Baldi, A.; Tribst, J.P.M.; Sarkis-Onofre, R.; Valandro, L.F.; Kleverlaan, C.J.; Scotti, N.; Pereira, G.K.R. Influence of CAD-CAM milling strategies on the outcome of indirect restorations: A scoping review. J. Prosthet. Dent. 2024, 131, 811.e1–811.e10. [CrossRef]
[31] Padrós, R.; Giner, L.; Herrero-Climent, M.; Falcao-Costa, C.; Ríos-Santos, J.V.; Gil, F.J. Influence of the CAD-CAM Systems on the Marginal Accuracy and Mechanical Properties of Dental Restorations. Int. J. Environ. Res. Public Health 2020, 17. [CrossRef] [PubMed]
[32] Sadid-Zadeh, R.; Li, R.; Miller, L.M.; Simon, M. Effect of Fabrication Technique on the Marginal Discrepancy and Resistance of Lithium Disilicate Crowns: An In Vitro Study. J. Prosthodont. 2019, 28, 1005–1010. [CrossRef] [PubMed]
[33] Alajaji, N.K.; Bardwell, D.; Finkelman, M.; Ali, A. Micro-CT Evaluation of Ceramic Inlays: Comparison of the Marginal and Internal Fit of Five and Three Axis CAM Systems with a Heat Press Technique. J. Esthet. Restor. Dent. 2017, 29, 49–58. [CrossRef]
[34] Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Marginal and internal fit of CAD-CAM inlay/onlay restorations: A systematic review of in vitro studies. J. Prosthet. Dent. 2019, 121, 590–597.e593. [CrossRef] [PubMed]
[35] Talic, R.; Alfadda, S.A. Internal Adaptation of Implant-Supported, Polymer-Infused Ceramic Crowns Fabricated by Two CAD/CAM Systems. J. Prosthodont. 2018, 27, 868–876. [CrossRef] [PubMed]
[36] Abduo, J.; Lyons, K.; Waddell, N.; Bennani, V.; Swain, M. A comparison of fit of CNC-milled titanium and zirconia frameworks to implants. Clin. Implant. Dent. Relat. Res. 2012, 14, e20–29. [CrossRef]
[37] Alghauli, M.A.; Wille, S.; Lehmann, F.; Kern, M. Survival and debonding resistance of posterior cantilever resin-bonded fixed dental prostheses for moderately and severely worn dentition during thermomechanical loading. Dent. Mater. 2023, 39, 634–639. [CrossRef] [PubMed]
[38] Kern, M. Fifteen-year survival of anterior all-ceramic cantilever resin-bonded fixed dental prostheses. J. Dent. 2017, 56, 133–135. [CrossRef]
[39] Hamid, N.F.A.; Ahmad, R. Computer-aided Design/Computer-aided Manufacturing (CAD/CAM) Machines With Scanning and Milling Capabilities for Fabricating Custom Posts and Cores: A Narrative Review. Malays. J. Med. Health Sci. 2022, 18, 166. [CrossRef]
[40] Beuer, F.; Neumeier, P.; Naumann, M. Marginal fit of 14-unit zirconia fixed dental prosthesis retainers. J. Oral. Rehabil. 2009, 36, 142–149. [CrossRef]
[41] Schaefer, O.; Kuepper, H.; Thompson, G.A.; Cachovan, G.; Hefti, A.F.; Guentsch, A. Effect of CNC-milling on the marginal and internal fit of dental ceramics: A pilot study. Dent. Mater. 2013, 29, 851–858. [CrossRef] [PubMed]
[42] Camargo, B.; Willems, E.; Jacobs, W.; Van Landuyt, K.; Peumans, M.; Zhang, F.; Vleugels, J.; Van Meerbeek, B. 3D printing and milling accuracy influence full-contour zirconia crown adaptation. Dent. Mater. 2022, 38, 1963–1976. [CrossRef] [PubMed]
[43] Zeltner, M.; Sailer, I.; Mühlemann, S.; Özcan, M.; Hämmerle, C.H.; Benic, G.I. Randomized controlled within-subject evaluation of digital and conventional workflows for the fabrication of lithium disilicate single crowns. Part III: Marginal and internal fit. J. Prosthet. Dent. 2017, 117, 354–362. [CrossRef] [PubMed]
[44] Bosch, G.; Ender, A.; Mehl, A. A 3-dimensional accuracy analysis of chairside CAD/CAM milling processes. J. Prosthet. Dent. 2014, 112, 1425–1431. [CrossRef]
[45] Kirsch, C.; Ender, A.; Attin, T.; Mehl, A. Trueness of four different milling procedures used in dental CAD/CAM systems. Clin. Oral. Investig. 2017, 21, 551–558. [CrossRef] [PubMed]
[46] Lawson, N.C.; Bansal, R.; Burgess, J.O. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent. Mater. 2016, 32, e275–e283. [CrossRef] [PubMed]
[47] Kim, J.H.; Cho, B.H.; Lee, J.H.; Kwon, S.J.; Yi, Y.A.; Shin, Y.; Roh, B.D.; Seo, D.G. Influence of preparation design on fit and ceramic thickness of CEREC 3 partial ceramic crowns after cementation. Acta Odontol. Scand. 2015, 73, 107–113. [CrossRef]
[48] de Paula Silveira, A.C.; Chaves, S.B.; Hilgert, L.A.; Ribeiro, A.P. Marginal and internal fit of CAD-CAM-fabricated composite resin and ceramic crowns scanned by 2 intraoral cameras. J. Prosthet. Dent. 2017, 117, 386–392. [CrossRef] [PubMed]
[49] Borba, M.; Cesar, P.F.; Griggs, J.A.; Della Bona, Á. Adaptation of all-ceramic fixed partial dentures. Dent. Mater. 2011, 27, 1119–1126. [CrossRef]
[50] Bae, S.Y.; Park, J.Y.; Jeong, I.D.; Kim, H.Y.; Kim, J.H.; Kim, W.C. Three-dimensional analysis of marginal and internal fit of copings fabricated with polyetherketoneketone (PEKK) and zirconia. J. Prosthodont. Res. 2017, 61, 106–112. [CrossRef]
[51] Kim, C.M.; Kim, S.R.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Trueness of milled prostheses according to number of ball-end mill burs. J. Prosthet. Dent. 2016, 115, 624–629. [CrossRef]
[52] Alfaro, D.P.; Ruse, N.D.; Carvalho, R.M.; Wyatt, C.C. Assessment of the Internal Fit of Lithium Disilicate Crowns Using Micro-CT. J. Prosthodont. 2015, 24, 381–386. [CrossRef] [PubMed]
[53] Dahl, B.E.; Rønold, H.J.; Dahl, J.E. Internal fit of single crowns produced by CAD-CAM and lost-wax metal casting technique assessed by the triple-scan protocol. J. Prosthet. Dent. 2017, 117, 400–404. [CrossRef]
[54] Boitelle, P.; Tapie, L.; Mawussi, B.; Fromentin, O. 3D fitting accuracy evaluation of CAD/CAM copings—Comparison with spacer design settings. Int. J. Comput. Dent. 2016, 19, 27–43. [PubMed]
[55] Karnakis, D.; Mortimer, V.; Knowles, M., "Recent advances in ultrafast laser micromachining systems for material micromanufacturing," In Proceedings of the 8th International Conference and Exhibition on Laser Metrology, Machine Tool, CMM & Robotic Performance, Cardif, Wales, 26–28 June 2007, 120–130.
[56] Caputi, A.; Russo, D. The optimization of the control logic of a redundant six axis milling machine. J. Intell. Manuf. 2021, 32, 1441–1453. [CrossRef]
[57] Atlas, A.; Isleem, W.; Bergler, M.; Fraiman, H.P.; Walter, R.; Lawson, N.D. Factors affecting the marginal fit of CAD-CAM restorations and concepts to improve outcomes. Curr. Oral Health Rep. 2019, 6, 277–283. [CrossRef]
[58] Jin, M.; Zhao, J.; Zheng, Y. Effects of Grinding and Polishing on Surface Characteristics of Monolithic Zirconia Fabricated by Different Manufacturing Processes: Wet Deposition and Dry Milling. J. Prosthodont. 2022, 31, 714–721. [CrossRef] [PubMed]
[59] Mourouzis, P.; Tolidis, K. Effects of milling method and artificial ageing on optical properties of high translucent zirconia for chairside restorations. Dent. Mater. 2022, 38, 108–120. [CrossRef] [PubMed]
[60] Shokrani, A.; Dhokia, V.; Newman, S.T. Environmentally conscious machining of difficult-to-machine materials with regard to cutting fluids. Int. J. Mach. Tools Manuf. 2012, 57, 83–101. [CrossRef]
[61] Kikuchi, M. The use of cutting temperature to evaluate the machinability of titanium alloys. Acta Biomater. 2009, 5, 770–775. [CrossRef]
[62] Fasbinder, D.J. Materials for chairside CAD/CAM restorations. Compend. Contin. Educ. Dent. 2010, 31, 702–709. [PubMed]
[63] Kwon, W.C.; Park, M.G. Evaluation of mechanical properties of dental zirconia in different milling conditions and sintering temperatures. J. Prosthet. Dent. 2023, 130, 909–916. [CrossRef] [PubMed]
[64] Denry, I.; Kelly, J.R. State of the art of zirconia for dental applications. Dent. Mater. 2008, 24, 299–307. [CrossRef] [PubMed]
[65] Rekow, D.; Thompson, V.P. Near-surface damage--a persistent problem in crowns obtained by computer-aided design and manufacturing. Proc. Inst. Mech. Eng. H 2005, 219, 233–243. [CrossRef]
[66] Wang, H.; Aboushelib, M.N.; Feilzer, A.J. Strength influencing variables on CAD/CAM zirconia frameworks. Dent. Mater. 2008, 24, 633–638. [CrossRef] [PubMed]
[67] Denkena, B.; Breidenstein, B.; Busemann, S.; Lehr, C.M. Impact of hard machining on zirconia based ceramics for dental applications. Procedia Cirp. 2017, 65, 248–252. [CrossRef]
[68] Ahmed, M.A.A.; Kern, M.; Mourshed, B.; Wille, S.; Chaar, M.S. Fracture resistance of maxillary premolars restored with different endocrown designs and materials after artificial ageing. J. Prosthodont. Res. 2022, 66, 141–150. [CrossRef]
[69] Gold, S.A.; Ferracane, J.L.; da Costa, J. Effect of Crystallization Firing on Marginal Gap of CAD/CAM Fabricated Lithium Disilicate Crowns. J. Prosthodont. 2018, 27, 63–66. [CrossRef] [PubMed]
[70] Sadan, A.; Blatz, M.B.; Lang, B. Clinical considerations for densely sintered alumina and zirconia restorations: Part 1. Int. J. Periodontics Restor. Dent. 2005, 25, 213–219.Available online: https://pubmed.ncbi.nlm.nih.gov/16089042/
[71] Song, X.F.; Ma, H.R.; He, Y.P.; Yin, L. Soft machining-induced surface and edge chipping damage in pre-crystalized lithium silicate glass ceramics. J. Mech. Behav. Biomed. Mater. 2022, 131. [CrossRef]
[72] Yan, Y.; Mao, Y.; Li, B.; Zhou, P. Machinability of the Thermoplastic Polymers: PEEK, PI, and PMMA. Polymers 2021, 13. [CrossRef]
[73] Beșliu, I.; Tamașag, I.; Slătineanu, L. Investigations on milling performance of Polyetheretherketone (PEEK). Preprint 2024, . [CrossRef]
[74] Chokaree, P.; Poovarodom, P.; Chaijareenont, P.; Yavirach, A.; Rungsiyakull, P. Biomaterials and Clinical Applications of Customized Healing Abutment—A Narrative Review. J. Funct. Biomater. 2022, 13. [CrossRef] [PubMed]
[75] Gonçalves, M.C.C.; Mergulhão, M.V.; Batalha, G.F.; Stoeterau, R.L., "Heat Treatment Influence on Micromilling of Additively Manufactured Titanium," In Proceedings of the Brazilian Manufacturing Engineering Congress, Brasilia, Brazil, 10–12 May 2023, 172–182. [CrossRef]
[76] Ahadian, S.; Finbloom, J.A.; Mofidfar, M.; Diltemiz, S.E.; Nasrollahi, F.; Davoodi, E.; Hosseini, V.; Mylonaki, I.; Sangabathuni, S.; Montazerian, H.; et al. Micro and nanoscale technologies in oral drug delivery. Adv. Drug Deliv. Rev. 2020, 157, 37–62. [CrossRef]
[77] Tamez-Tamez, J.I.; Vázquez-Lepe, E.; Rodriguez, C.A.; Martínez-López, J.I.; García-López, E. Assessment of geometrical dimensions and puncture feasibility of microneedles manufactured by micromilling. Int. J. Adv. Manuf. Technol. 2023, 126, 4983–4996. [CrossRef]
[78] Cappellini, C.; Malandruccolo, A.; Abeni, A.; Attanasio, A. A feasibility study of promoting osseointegration surface roughness by micro-milling of Ti-6Al-4V biomedical alloy. Int. J. Adv. Manuf. Technol. 2023, 126, 3053–3067. [CrossRef]
[79] Al-Shibaany, Z.Y.A.; Penchev, P.; Hedley, J.; Dimov, S. Laser Micromachining of Lithium Niobate-Based Resonant Sensors towards Medical Devices Applications. Sensors 2020, 20. [CrossRef] [PubMed]
[80] Chang, F.-Y.; Liang, T.-H.; Wu, T.-J.; Wu, C.-H. Using 3D printing and femtosecond laser micromachining to fabricate biodegradable peripheral vascular stents with high structural uniformity and dimensional precision. Int. J. Adv. Manuf. Technol. 2021, 116, 1523–1536. [CrossRef]
[81] Hart, C.; Rajaraman, S. Low-Power, Multimodal Laser Micromachining of Materials for Applications in sub-5 µm Shadow Masks and sub-10 µm Interdigitated Electrodes (IDEs) Fabrication. Micromachines 2020, 11. [CrossRef]
[82] Faeda, R.S.; Tavares, H.S.; Sartori, R.; Guastaldi, A.C.; Marcantonio, E. Evaluation of titanium implants with surface modification by laser beam: Biomechanical study in rabbit tibias. Braz. Oral Res. 2009, 23, 137–143. [CrossRef]
[83] Hallgren, C.; Reimers, H.; Chakarov, D.; Gold, J.; Wennerberg, A. An in vivo study of bone response to implants topographically modified by laser micromachining. Biomaterials 2003, 24, 701–710. [CrossRef] [PubMed]
[84] Anselme, K.; Bigerelle, M. Role of materials surface topography on mammalian cell response. Int. Mater. Rev. 2011, 56, 243–266. [CrossRef]
[85] Martinez, E.; Engel, E.; Planell, J.; Samitier, J. Effects of artificial micro-and nano-structured surfaces on cell behaviour. Ann. Anat.-Anat. Anz. 2009, 191, 126–135. [CrossRef]
[86] Györgyey, Á.; Ungvári, K.; Kecskeméti, G.; Kopniczky, J.; Hopp, B.; Oszkó, A.; Pelsöczi, I.; Rakonczay, Z.; Nagy, K.; Turzó, K. Attachment and proliferation of human osteoblast-like cells (MG-63) on laser-ablated titanium implant material. Mater. Sci. Eng. C 2013, 33, 4251–4259. [CrossRef]
[87] Zwahr, C.; Günther, D.; Brinkmann, T.; Gulow, N.; Oswald, S.; Grosse Holthaus, M.; Lasagni, A.F. Laser surface pattering of titanium for improving the biological performance of dental implants. Adv. Healthc. Mater. 2017, 6, 1600858. [CrossRef]
[88] Skoog, S.A.; Kumar, G.; Narayan, R.J.; Goering, P.L. Biological responses to immobilized microscale and nanoscale surface topographies. Pharmacol. Ther. 2018, 182, 33–55. [CrossRef] [PubMed]
[89] Carvalho, A.; Cangueiro, L.; Oliveira, V.; Vilar, R.; Fernandes, M.H.; Monteiro, F.J. Femtosecond laser microstructured Alumina toughened Zirconia: A new strategy to improve osteogenic differentiation of hMSCs. Appl. Surf. Sci. 2018, 435, 1237–1245. [CrossRef]
[90] Hirota, M.; Harai, T.; Ishibashi, S.; Mizutani, M.; Hayakawa, T. Cortical bone response toward nanosecond-pulsed laser-treated zirconia implant surfaces. Dent. Mater. J. 2019, 38, 444–451. [CrossRef] [PubMed]
[91] Cunha, A.; Elie, A.-M.; Plawinski, L.; Serro, A.P.; Botelho do Rego, A.M.; Almeida, A.; Urdaci, M.C.; Durrieu, M.-C.; Vilar, R. Femtosecond laser surface texturing of titanium as a method to reduce the adhesion of Staphylococcus aureus and biofilm formation. Appl. Surf. Sci. 2016, 360, 485–493. [CrossRef]
[92] Tijing, L.D.; Ruelo, M.T.G.; Amarjargal, A.; Pant, H.R.; Park, C.-H.; Kim, D.W.; Kim, C.S. Antibacterial and superhydrophilic electrospun polyurethane nanocomposite fibers containing tourmaline nanoparticles. Chem. Eng. J. 2012, 197, 41–48. [CrossRef]
[93] Lutey, A.H.; Gemini, L.; Romoli, L.; Lazzini, G.; Fuso, F.; Faucon, M.; Kling, R. Towards laser-textured antibacterial surfaces. Sci. Rep. 2018, 8. [CrossRef]
[94] Liu, M.; Zhou, J.; Yang, Y.; Zheng, M.; Yang, J.; Tan, J. Surface modification of zirconia with polydopamine to enhance fibroblast response and decrease bacterial activity in vitro: A potential technique for soft tissue engineering applications. Colloids Surf. B Biointerfaces 2015, 136, 74–83. [CrossRef] [PubMed]
[95] Çelen, S.; Özden, H. Laser-induced novel patterns: As smart strain actuators for new-age dental implant surfaces. Appl. Surf. Sci. 2012, 263, 579–585. [CrossRef]
[96] Man, H.C.; Wang, Q.; Guo, X. Laser surface microdrilling of Ti and laser gas nitrided Ti for enhancing fixation of dental implants. Opt. Lasers Eng. 2010, 48, 583–588. [CrossRef]
[97] Yu, P.; Wang, X.Y. Effects of Surface Treatment Procedures on Bond Strength of Lithium Disilicate Glass Ceramic. Chin. J. Dent. Res. 2021, 24, 119–124. [CrossRef]
[98] Zhang, X.; Liang, W.; Jiang, F.; Wang, Z.; Zhao, J.; Zhou, C.; Wu, J. Effects of air-abrasion pressure on mechanical and bonding properties of translucent zirconia. Clin. Oral Investig. 2021, 25, 1979–1988. [CrossRef] [PubMed]
[99] Souza, J.C.M.; Raffaele-Esposito, A.; Carvalho, O.; Silva, F.; Özcan, M.; Henriques, B. Surface modification of zirconia or lithium disilicate-reinforced glass ceramic by laser texturing to increase the adhesion of prosthetic surfaces to resin cements: An integrative review. Clin. Oral Investig. 2023, 27, 3331–3345. [CrossRef]
[100] Sahoo, N.; Carvalho, O.; Özcan, M.; Silva, F.; Souza, J.C.M.; Lasagni, A.F.; Henriques, B. Ultrashort pulse laser patterning of zirconia (3Y-TZP) for enhanced adhesion to resin-matrix cements used in dentistry: An integrative review. J. Mech. Behav. Biomed. Mater. 2023, 143. [CrossRef] [PubMed]
[101] Li, Q.; Li, C.; Wang, Y. Effect of femtosecond laser ablate ultra-fine microgrooves on surface properties of dental zirconia materials. J. Mech. Behav. Biomed. Mater. 2022, 134. [CrossRef]
[102] Alayad, A. Influence of lithium disilicate pretreatment using photodynamic therapy, non-thermal plasma, and laser treatment on surface roughness and bond strength. Photodiagnosis. Photodyn. Ther. 2023, 42, 103512. [CrossRef]
[103] Tokar, E.; Polat, S.; Ozturk, C. Repair bond strength of composite to Er,Cr:YSGG laser irradiated zirconia and porcelain surfaces. Biomed. J. 2019, 42, 193–199. [CrossRef]
[104] Chavali, R.; Nejat, A.H.; Lawson, N.C. Machinability of CAD-CAM materials. J. Prosthet. Dent. 2017, 118, 194–199. [CrossRef]
[105] Saker, S.; Alqutaibi, A.Y.; Alghauli, M.A.; Hashem, D.; Borzangy, S.; Farghal, A.E.; Alnazzawi, A.A.; Ainoosah, S.; AbdElaziz, M.H. The Influence of Ferrule Design and Pulpal Extensions on the Accuracy of Fit and the Fracture Resistance of Zirconia-Reinforced Lithium Silicate Endocrowns. Materials 2024, 17. [CrossRef] [PubMed]
[106] Facenda, J.C.; Borba, M.; Corazza, P.H. A literature review on the new polymer-infiltrated ceramic-network material (PICN). J. Esthet. Restor. Dent. 2018, 30, 281–286. [CrossRef]
[107] Seo, D.; Yi, Y.; Roh, B. The effect of preparation designs on the marginal and internal gaps in Cerec3 partial ceramic crowns. J. Dent. 2009, 37, 374–382. [CrossRef] [PubMed]
[108] Guess, P.C.; Vagkopoulou, T.; Zhang, Y.; Wolkewitz, M.; Strub, J.R. Marginal and internal fit of heat pressed versus CAD/CAM fabricated all-ceramic onlays after exposure to thermo-mechanical fatigue. J. Dent. 2014, 42, 199–209. [CrossRef] [PubMed]
[109] Hamza, T.A.; Ezzat, H.A.; El-Hossary, M.M.; Katamish, H.A.; Shokry, T.E.; Rosenstiel, S.F. Accuracy of ceramic restorations made with two CAD/CAM systems. J. Prosthet. Dent. 2013, 109, 83–87. [CrossRef]
[110] Spitznagel, F.A.; Boldt, J.; Gierthmuehlen, P.C. CAD/CAM Ceramic Restorative Materials for Natural Teeth. J. Dent. Res. 2018, 97, 1082–1091. [CrossRef] [PubMed]
[111] Alghauli, M.; Alqutaibi, A.Y.; Wille, S.; Kern, M. Clinical outcomes and influence of material parameters on the behavior and survival rate of thin and ultrathin occlusal veneers: A systematic review. J. Prosthodont. Res. 2023, 67, 45–54. [CrossRef]
[112] Schlichting, L.H.; Resende, T.H.; Reis, K.R.; Raybolt Dos Santos, A.; Correa, I.C.; Magne, P. Ultrathin CAD-CAM glass-ceramic and composite resin occlusal veneers for the treatment of severe dental erosion: An up to 3-year randomized clinical trial. J. Prosthet. Dent. 2022, 128, 158.e151–158.e112. [CrossRef] [PubMed]
[113] Oudkerk, J.; Eldafrawy, M.; Bekaert, S.; Grenade, C.; Vanheusden, A.; Mainjot, A. The one-step no-prep approach for full-mouth rehabilitation of worn dentition using PICN CAD-CAM restorations: 2-yr results of a prospective clinical study. J. Dent. 2020, 92, 103245. [CrossRef] [PubMed]
[114] Becker, M.; Chaar, M.S.; Kern, M. Resin-bonded attachments made of monolithic zirconia ceramic: A minimally invasive and esthetic treatment approach. Quintessence Int. 2023, 54, 220–226. [CrossRef] [PubMed]
[115] McLean, J.W.; von Fraunhofer, J.A. The estimation of cement film thickness by an in vivo technique. Br Dent J 1971, 131, 107–111. [CrossRef] [PubMed]
[116] Tan, P.L.; Gratton, D.G.; Diaz-Arnold, A.M.; Holmes, D.C. An in vitro comparison of vertical marginal gaps of CAD/CAM titanium and conventional cast restorations. J. Prosthodont. 2008, 17, 378–383. [CrossRef]
[117] Han, H.S.; Yang, H.S.; Lim, H.P.; Park, Y.J. Marginal accuracy and internal fit of machine-milled and cast titanium crowns. J. Prosthet. Dent. 2011, 106, 191–197. [CrossRef] [PubMed]
[118] Matsumura, M.; Nozaki, K.; Yanaka, W.; Nemoto, R.; Takita, M.; Yamashita, K.; Matsumura, M.; Miura, H. Optimization of milling condition of composite resin blocks for CAD/CAM to improve surface roughness and flexural strength. Dent. Mater. J. 2020, 39, 1057–1063. [CrossRef]
[119] Wang, W.; Yu, H.; Liu, Y.; Jiang, X.; Gao, B. Trueness analysis of zirconia crowns fabricated with 3-dimensional printing. J. Prosthet. Dent. 2019, 121, 285–291. [CrossRef]
[120] Lee, K.B.; Park, C.W.; Kim, K.H.; Kwon, T.Y. Marginal and internal fit of all-ceramic crowns fabricated with two different CAD/CAM systems. Dent. Mater. J. 2008, 27, 422–426. [CrossRef]
[121] Baig, M.R.; Tan, K.B.; Nicholls, J.I. Evaluation of the marginal fit of a zirconia ceramic computer-aided machined (CAM) crown system. J. Prosthet. Dent. 2010, 104, 216–227. [CrossRef]
[122] Grenade, C.; Mainjot, A.; Vanheusden, A. Fit of single tooth zirconia copings: Comparison between various manufacturing processes. J. Prosthet. Dent. 2011, 105, 249–255. [CrossRef] [PubMed]
[123] Sulaiman, F.; Chai, J.; Jameson, L.M.; Wozniak, W.T. A comparison of the marginal fit of In-Ceram, IPS Empress, and Procera crowns. Int. J. Prosthodont. 1997, 10, 478–484. [PubMed]
[124] Karataşli, O.; Kursoğlu, P.; Capa, N.; Kazazoğlu, E. Comparison of the marginal fit of different coping materials and designs produced by computer aided manufacturing systems. Dent. Mater. J. 2011, 30, 97–102. [CrossRef]
[125] Rinke, S.; Fornefett, D.; Gersdorff, N.; Lange, K.; Roediger, M. Multifactorial analysis of the impact of different manufacturing processes on the marginal fit of zirconia copings. Dent. Mater. J. 2012, 31, 601–609. [CrossRef] [PubMed]
[126] May, K.B.; Russell, M.M.; Razzoog, M.E.; Lang, B.R. Precision of fit: The Procera AllCeram crown. J. Prosthet. Dent. 1998, 80, 394–404. [CrossRef] [PubMed]
[127] Beschnidt, S.M.; Strub, J.R. Evaluation of the marginal accuracy of different all-ceramic crown systems after simulation in the artificial mouth. J. Oral. Rehabil. 1999, 26, 582–593. [CrossRef]
[128] Boening, K.W.; Wolf, B.H.; Schmidt, A.E.; Kästner, K.; Walter, M.H. Clinical fit of Procera AllCeram crowns. J. Prosthet. Dent. 2000, 84, 419–424. [CrossRef] [PubMed]
[129] Yeo, I.S.; Yang, J.H.; Lee, J.B. In vitro marginal fit of three all-ceramic crown systems. J. Prosthet. Dent. 2003, 90, 459–464. [CrossRef] [PubMed]
[130] Coli, P.; Karlsson, S. Precision of a CAD/CAM technique for the production of zirconium dioxide copings. Int. J. Prosthodont. 2004, 17, 577–580. [CrossRef]
[131] Balkaya, M.C.; Cinar, A.; Pamuk, S. Influence of firing cycles on the margin distortion of 3 all-ceramic crown systems. J. Prosthet. Dent. 2005, 93, 346–355. [CrossRef]
[132] Beuer, F.; Aggstaller, H.; Edelhoff, D.; Gernet, W.; Sorensen, J. Marginal and internal fits of fixed dental prostheses zirconia retainers. Dent. Mater. 2009, 25, 94–102. [CrossRef]
[133] Quintas, A.F.; Oliveira, F.; Bottino, M.A. Vertical marginal discrepancy of ceramic copings with different ceramic materials, finish lines, and luting agents: An in vitro evaluation. J. Prosthet. Dent. 2004, 92, 250–257. [CrossRef]
[134] Lüchtenborg, J.; Willems, E.; Zhang, F.; Wesemann, C.; Weiss, F.; Nold, J.; Sun, J.; Sandra, F.; Bai, J.; Reveron, H.; et al. Accuracy of additively manufactured zirconia four-unit fixed dental prostheses fabricated by stereolithography, digital light processing and material jetting compared with subtractive manufacturing. Dent. Mater. 2022, 38, 1459–1469. [CrossRef] [PubMed]
[135] Suárez, M.J.; González de Villaumbrosia, P.; Pradíes, G.; Lozano, J.F. Comparison of the marginal fit of Procera AllCeram crowns with two finish lines. Int. J. Prosthodont. 2003, 16, 229–232.Available online: http://43.230.198.52/216/IJP/2003/june/2.pdf
[136] Suominen, J.M.; Frankberg, E.J.; Vallittu, P.K.; Levänen, E.; Vihinen, J.; Vastamäki, T.; Kari, R.; Lassila, L.V. Three-dimensional printing of zirconia: Characterization of early stage material properties. Biomater. Investig. Dent. 2019, 6, 23–31. [CrossRef]
[137] Manière, C.; Kerbart, G.; Harnois, C.; Marinel, S. Modeling sintering anisotropy in ceramic stereolithography of silica. Acta Mater. 2020, 182, 163–171. [CrossRef]
[138] Patzelt, S.B.; Spies, B.C.; Kohal, R.J. CAD/CAM-fabricated implant-supported restorations: A systematic review. Clin. Oral Implants Res. 2015, 26, 77–85. [CrossRef]
[139] Panchal, M.; Khare, S.; Khamkar, P.; Suresh Bhole, K. Dental implants: A review of types, design analysis, materials, additive manufacturing methods, and future scope. Mater. Today Proc. 2022, 68, 1860–1867. [CrossRef]
[140] D’Souza, K.M.; Aras, M.A. Applications of CAD/CAM Technology in Dental Implant Planning and Implant Surgery. Advances in Dental Implantology using Nanomaterials and Allied Technology Applications ; Springer: Cham, Switzerland, 2021; 247–286. . [CrossRef]
[141] Turkyilmaz, I.; Eskow, C.C.; Soganci, G.; Turkyilmaz, I.; Eskow, C.C.; Soganci, G. CAD/CAM Technology in Implant Dentistry. Current Concepts in Dental Implantology ; IntechOpen: London, UK, 2015; . . [CrossRef]
[142] Abduo, J. Fit of CAD/CAM Implant Frameworks: A Comprehensive Review. J. Oral Implantol. 2014, 40, 758–766. [CrossRef] [PubMed]
[143] Smeets, R.; Stadlinger, B.; Schwarz, F.; Beck-Broichsitter, B.; Jung, O.; Precht, C.; Kloss, F.; Gröbe, A.; Heiland, M.; Ebker, T. Impact of Dental Implant Surface Modifications on Osseointegration. Biomed. Res. Int. 2016, 2016. [CrossRef]
[144] Yüzügüllü, B.; Avci, M. The implant-abutment interface of alumina and zirconia abutments. Clin. Implant Dent. Relat. Res. 2008, 10, 113–121. [CrossRef] [PubMed]
[145] Vigolo, P.; Fonzi, F.; Majzoub, Z.; Cordioli, G. An in vitro evaluation of titanium, zirconia, and alumina procera abutments with hexagonal connection. Int. J. Oral Maxillofac. Implants 2006, 21, 575–580.Available online: https://www.researchgate.net/publication/6833930_An_in_vitro_evaluation_of_titanium_zirconia_and_alumina_Procera_abutments_with_hexagonal_connection
[146] Sierraalta, M.; Vivas, J.L.; Razzoog, M.E.; Wang, R.F. Precision of fit of titanium and cast implant frameworks using a new matching formula. Int. J. Dent. 2012, 2012, 374315. [CrossRef] [PubMed]
[147] Jemt, T.; Bäck, T.; Petersson, A. Precision of CNC-milled titanium frameworks for implant treatment in the edentulous jaw. Int. J. Prosthodont. 1999, 12, 209–215.Available online: https://pubmed.ncbi.nlm.nih.gov/10635187/
[148] Fernández, M.; Delgado, L.; Molmeneu, M.; García, D.; Rodríguez, D. Analysis of the misfit of dental implant-supported prostheses made with three manufacturing processes. J. Prosthet. Dent. 2014, 111, 116–123. [CrossRef]
[149] Nassar, H.I.; Fateen, A. Accuracy of fit for cobaltchromium bar over two implants fabricated with different manufacturing techniques: An in-vitro study. BMC Oral Health 2023, 23. [CrossRef] [PubMed]
[150] AlRasheed, F.; AlWazzan, K. The effect of framework fabrication technique on the fit accuracy of full arch screw retained implant supported prostheses. Saudi Dent. J. 2022, 34, 288–297. [CrossRef] [PubMed]
[151] de França, D.G.; Morais, M.H.; das Neves, F.D.; Barbosa, G.A. Influence of CAD/CAM on the fit accuracy of implant-supported zirconia and cobalt-chromium fixed dental prostheses. J. Prosthet. Dent. 2015, 113, 22–28. [CrossRef] [PubMed]
[152] Alshehri, H.A.; Altaweel, S.M.; Alshaibani, R.; Alahmari, E.A.; Alotaibi, H.N.; Alfouzan, A.F.; Labban, N. Effect of Different Wax Pattern Manufacturing Techniques on the Marginal Fit of Lithium Disilicate Crowns. Materials 2022, 15. [CrossRef] [PubMed]
[153] Herrera, S.P.; Merchant, V.A. Dimensional stability of dental impressions after immersion disinfection. J. Am. Dent. Assoc. 1986, 113, 419–422. [CrossRef]
[154] Johansen, R.E.; Stackhouse, J.A. Dimensional changes of elastomers during cold sterilization. J. Prosthet. Dent. 1987, 57, 233–236. [CrossRef] [PubMed]
[155] Miyazaki, T.; Hotta, Y. CAD/CAM systems available for the fabrication of crown and bridge restorations. Aust. Dent. J. 2011, 56, 97–106. [CrossRef]
[156] Shamseddine, L.; Mortada, R.; Rifai, K.; Chidiac, J.J. Fit of pressed crowns fabricated from two CAD-CAM wax pattern process plans: A comparative in vitro study. J. Prosthet. Dent. 2017, 118, 49–54. [CrossRef] [PubMed]
[157] Homsy, F.R.; Özcan, M.; Khoury, M.; Majzoub, Z.A.K. Comparison of fit accuracy of pressed lithium disilicate inlays fabricated from wax or resin patterns with conventional and CAD-CAM technologies. J. Prosthet. Dent. 2018, 120, 530–536. [CrossRef] [PubMed]
[158] Homsy, F.R.; Özcan, M.; Khoury, M.; Majzoub, Z.A.K. Marginal and internal fit of pressed lithium disilicate inlays fabricated with milling, 3D printing, and conventional technologies. J. Prosthet. Dent. 2018, 119, 783–790. [CrossRef] [PubMed]
[159] Ali Majeed, Z.; Hasan Jasim, H. Digital Evaluation of Trueness and Fitting Accuracy of Co-Cr Crown Copings Fabricated by Different Manufacturing Technologies. Cureus 2023, 15, e39819. [CrossRef]
[160] Jeong, Y.G.; Lee, W.S.; Lee, K.B. Accuracy evaluation of dental models manufactured by CAD/CAM milling method and 3D printing method. J. Adv. Prosthodont. 2018, 10, 245–251. [CrossRef]
[161] Alshawaf, B.; Weber, H.P.; Finkelman, M.; El Rafie, K.; Kudara, Y.; Papaspyridakos, P. Accuracy of printed casts generated from digital implant impressions versus stone casts from conventional implant impressions: A comparative in vitro study. Clin. Oral Implants Res. 2018, 29, 835–842. [CrossRef]
[162] Yau, H.; Yang, T.; Lin, Y. Comparison of 3-D Printing and 5-axis Milling for the Production of Dental e-models from Intra-oral Scanning. Comput.-Aided Des. Appl. 2016, 13, 32–38. [CrossRef]
[163] Choi, J.W.; Ahn, J.J.; Son, K.; Huh, J.B. Three-Dimensional Evaluation on Accuracy of Conventional and Milled Gypsum Models and 3D Printed Photopolymer Models. Materials 2019, 12. [CrossRef]
[164] Sidhom, M.; Zaghloul, H.; Mosleh, I.E.; Eldwakhly, E. Effect of Different CAD/CAM Milling and 3D Printing Digital Fabrication Techniques on the Accuracy of PMMA Working Models and Vertical Marginal Fit of PMMA Provisional Dental Prosthesis: An In Vitro Study. Polymers 2022, 14. [CrossRef]
[165] Akl, M.A.; Stendahl, C.G. Removable partial denture frameworks in the age of digital dentistry: A review of the literature. Prosthesis 2022, 4, 184–201. [CrossRef]
[166] Arnold, C.; Hey, J.; Schweyen, R.; Setz, J.M. Accuracy of CAD-CAM-fabricated removable partial dentures. J. Prosthet. Dent. 2018, 119, 586–592. [CrossRef] [PubMed]
[167] Piao, X.Y.; Jeon, J.; Shim, J.S.; Park, J.M. A Digital Workflow for the Fabrication of a Milled Removable Partial Denture. Int. J. Environ. Res. Public Health 2022, 19. [CrossRef] [PubMed]
[168] Snosi, A.M.; Lotfy, S.M.; Thabet, Y.G.; Sabet, M.E.; Rizk, F.N. Subtractive versus additive indirect manufacturing techniques of digitally designed partial dentures. J. Adv. Prosthodont. 2021, 13, 327–332. [CrossRef] [PubMed]
[169] Oh, K.C.; Yun, B.S.; Kim, J.H. Accuracy of metal 3D printed frameworks for removable partial dentures evaluated by digital superimposition. Dent. Mater. 2022, 38, 309–317. [CrossRef]
[170] Muehlemann, E.; Özcan, M. Accuracy of Removable Partial Denture Frameworks Fabricated Using Conventional and Digital Technologies. Eur. J. Prosthodont. Restor. Dent. 2022, 30, 76–86. [CrossRef]
[171] Soltanzadeh, P.; Suprono, M.S.; Kattadiyil, M.T.; Goodacre, C.; Gregorius, W. An In Vitro Investigation of Accuracy and Fit of Conventional and CAD/CAM Removable Partial Denture Frameworks. J. Prosthodont. 2019, 28, 547–555. [CrossRef]
[172] Ahmed, N.; Abbasi, M.S.; Haider, S.; Ahmed, N.; Habib, S.R.; Altamash, S.; Zafar, M.S.; Alam, M.K. Fit Accuracy of Removable Partial Denture Frameworks Fabricated with CAD/CAM, Rapid Prototyping, and Conventional Techniques: A Systematic Review. Biomed. Res. Int. 2021, 2021. [CrossRef] [PubMed]
[173] Ohkubo, C.; Watanabe, I.; Ford, J.P.; Nakajima, H.; Hosoi, T.; Okabe, T. The machinability of cast titanium and Ti-6Al-4V. Biomaterials 2000, 21, 421–428. [CrossRef] [PubMed]
[174] Ohkubo, C.; Hosoi, T.; Ford, J.P.; Watanabe, I. Effect of surface reaction layer on grindability of cast titanium alloys. Dent. Mater. 2006, 22, 268–274. [CrossRef]
[175] Ansari, I.H. Establishing the posterior palatal seal during the final impression stage. J. Prosthet. Dent. 1997, 78, 324–326. [CrossRef]
[176] Jacobson, T.E.; Krol, A.J. A contemporary review of the factors involved in complete dentures. Part III: Support. J. Prosthet. Dent. 1983, 49, 306–313. [CrossRef] [PubMed]
[177] Jacobson, T.E.; Krol, A.J. A contemporary review of the factors involved in complete dentures. Part II: Stability. J. Prosthet. Dent. 1983, 49, 165–172. [CrossRef] [PubMed]
[178] Jacobson, T.E.; Krol, A.J. A contemporary review of the factors involved in complete denture retention, stability, and support. Part I: Retention. J. Prosthet. Dent. 1983, 49, 5–15. [CrossRef] [PubMed]
[179] Yamamoto, S.; Kanazawa, M.; Iwaki, M.; Jokanovic, A.; Minakuchi, S. Effects of offset values for artificial teeth positions in CAD/CAM complete denture. Comput. Biol. Med. 2014, 52, 1–7. [CrossRef]
[180] Wang, C.; Shi, Y.F.; Xie, P.J.; Wu, J.H. Accuracy of digital complete dentures: A systematic review of in vitro studies. J. Prosthet. Dent. 2021, 125, 249–256. [CrossRef] [PubMed]
[181] Kim, C.M.; Jeon, J.H.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Three-dimensional evaluation of the reproducibility of presintered zirconia single copings fabricated with the subtractive method. J. Prosthet. Dent. 2016, 116, 237–241. [CrossRef] [PubMed]
[182] Hwang, H.J.; Lee, S.J.; Park, E.J.; Yoon, H.I. Assessment of the trueness and tissue surface adaptation of CAD-CAM maxillary denture bases manufactured using digital light processing. J. Prosthet. Dent. 2019, 121, 110–117. [CrossRef] [PubMed]
[183] Srinivasan, M.; Kamnoedboon, P.; McKenna, G.; Angst, L.; Schimmel, M.; Özcan, M.; Müller, F. CAD-CAM removable complete dentures: A systematic review and meta-analysis of trueness of fit, biocompatibility, mechanical properties, surface characteristics, color stability, time-cost analysis, clinical and patient-reported outcomes. J. Dent. 2021, 113, 103777. [CrossRef]
[184] Janeva, N.M.; Kovacevska, G.; Elencevski, S.; Panchevska, S.; Mijoska, A.; Lazarevska, B. Advantages of CAD/CAM versus Conventional Complete Dentures—A Review. Open Access Maced. J. Med. Sci. 2018, 6, 1498–1502. [CrossRef]
[185] de Oliveira Limírio, J.P.J.; Gomes, J.M.L.; Alves Rezende, M.C.R.; Lemos, C.A.A.; Rosa, C.; Pellizzer, E.P. Mechanical properties of polymethyl methacrylate as a denture base: Conventional versus CAD-CAM resin—A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2022, 128, 1221–1229. [CrossRef]
[186] Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J Prosthodont 2020, 29, 524–528. [CrossRef] [PubMed]
[187] Goodacre, B.J.; Goodacre, C.J.; Baba, N.Z.; Kattadiyil, M.T. Comparison of denture tooth movement between CAD-CAM and conventional fabrication techniques. J. Prosthet. Dent. 2018, 119, 108–115. [CrossRef] [PubMed]
[188] Murat, S.; Alp, G.; Alatalı, C.; Uzun, M. In Vitro Evaluation of Adhesion of Candida albicans on CAD/CAM PMMA-Based Polymers. J. Prosthodont. 2019, 28, e873–e879. [CrossRef]
[189] Al-Fouzan, A.F.; Al-Mejrad, L.A.; Albarrag, A.M. Adherence of Candida to complete denture surfaces in vitro: A comparison of conventional and CAD/CAM complete dentures. J. Adv. Prosthodont. 2017, 9, 402–408. [CrossRef]
[190] Tzanakakis, E.G.; Pandoleon, P.; Sarafianou, A.; Kontonasaki, E. Adhesion of Conventional, 3D-Printed and Milled Artificial Teeth to Resin Substrates for Complete Dentures: A Narrative Review. Polymers 2023, 15. [CrossRef]
[191] Davidowitz, G.; Kotick, P.G. The use of CAD/CAM in dentistry. Dent. Clin. N. Am. 2011, 55, 559–570. [CrossRef]
[192] Lerner, H.; Nagy, K.; Pranno, N.; Zarone, F.; Admakin, O.; Mangano, F. Trueness and precision of 3D-printed versus milled monolithic zirconia crowns: An in vitro study. J. Dent. 2021, 113, 103792. [CrossRef] [PubMed]
[193] Strub, J.R.; Rekow, E.D.; Witkowski, S. Computer-aided design and fabrication of dental restorations: Current systems and future possibilities. J. Am. Dent. Assoc. 2006, 137, 1289–1296. [CrossRef]
[194] Bae, E.J.; Jeong, I.D.; Kim, W.C.; Kim, J.H. A comparative study of additive and subtractive manufacturing for dental restorations. J. Prosthet. Dent. 2017, 118, 187–193. [CrossRef] [PubMed]
[195] Abualsaud, R.; Abussaud, M.; Assudmi, Y.; Aljoaib, G.; Khaled, A.; Alalawi, H.; Akhtar, S.; Matin, A.; Gad, M.M. Physiomechanical and Surface Characteristics of 3D-Printed Zirconia: An In Vitro Study. Materials 2022, 15. [CrossRef]
[196] Branco, A.C.; Colaço, R.; Figueiredo-Pina, C.G.; Serro, A.P. Recent Advances on 3D-Printed Zirconia-Based Dental Materials: A Review. Materials 2023, 16. [CrossRef] [PubMed]
[197] Meland, A.; Tollefors, C. Chair-Side Fabrication of Customized Interim Prostheses Using Additive Manufacturing—A Descriptive Study. Student thesis, Malmö högskola/Odontologiska Fakulteten. 2016 Available online: https://www.diva-portal.org/smash/record.jsf?pid=diva2%3A1479553 (accessed on 14 November 2024).
[198] Luthardt, R.G.; Holzhüter, M.S.; Rudolph, H.; Herold, V.; Walter, M.H. CAD/CAM-machining effects on Y-TZP zirconia. Dent. Mater. 2004, 20, 655–662. [CrossRef] [PubMed]
[199] Pour, R.; Randelzhofer, P.; Edelhoff, D.; Prandtner, O.; Rafael, C.; Liebermann, A. Innovative single-tooth replacement with an individual root-analog hybrid implant in the esthetic zone: Case report. Int. J. Oral Maxillofac. Implant 2017, 32, e153–e160. [CrossRef]
[200] Zhang, K.; Van Le, Q. Bioactive glass coated zirconia for dental implants: A review. J. Compos. Compd. 2020, 2, 10–17. [CrossRef]
[201] Pragana, J.P.M.; Sampaio, R.F.V.; Bragança, I.M.F.; Silva, C.M.A.; Martins, P.A.F. Hybrid metal additive manufacturing: A state–of–the-art review. Adv. Ind. Manuf. Eng. 2021, 2, 100032. [CrossRef]
[202] Imad, M.; Hosseini, A.; Kishawy, H.A. Optimization Methodologies in Intelligent Machining Systems—A Review. IFAC-PapersOnLine 2019, 52, 282–287. [CrossRef]
[203] Chen, M.; Wang, C.; An, Q.; Ming, W. Tool path strategy and cutting process monitoring in intelligent machining. Front. Mech. Eng. 2018, 13, 232–242. [CrossRef]
[204] Rahman, M.A.; Saleh, T.; Jahan, M.P.; McGarry, C.; Chaudhari, A.; Huang, R.; Tauhiduzzaman, M.; Ahmed, A.; Mahmud, A.A.; Bhuiyan, M.S.; et al. Review of Intelligence for Additive and Subtractive Manufacturing: Current Status and Future Prospects. Micromachines 2023, 14. [CrossRef]
[205] Zhang, J.; Starly, B.; Cai, Y.; Cohen, P.H.; Lee, Y.-S. Particle learning in online tool wear diagnosis and prognosis. J. Manuf. Process. 2017, 28, 457–463. [CrossRef]
We use cookies to improve your experience on our site. By continuing to use our site, you accept our use of cookies. Learn more